VA Disability Benefits for Secondary Conditions to Depression

CCK Law: Our Vital Role in Veterans Law
Depression is a mental health condition that can often manifest several secondary conditions. The combination of depression and secondary conditions can significantly impact a veteran’s well-being. Veterans who develop a condition that is secondary to their service-connected depression are eligible to receive VA disability benefits for their secondary condition.
What is Depression?
Depression, or major depressive disorder, is a serious medical condition that can interfere with necessary activities of life, such as eating, sleeping, and working. Depression can affect how a person feels and thinks. As such, depression often takes a significant mental, emotional, and physical toll on a person.
Symptoms of Depression
- Feelings of sadness, fatigue, worthlessness, guilt, or hopelessness
- Loss of interest or pleasure in usual activities
- Disturbances in sleep
- Anxiety or restlessness
- Irritability
- Difficulty concentrating or remembering things
- Loss of appetite and weight loss or increased appetite and weight gain
- Thoughts of death or suicide

What Causes Depression in Veterans?
Rates of depression are particularly high among servicemembers and veterans. A 2014 study found that nearly 1 in 4 active duty servicemembers showed signs of a mental health condition.
The Substance Abuse and Mental Health Services Administration also determined that approximately 18.5 percent of veterans returning from Iraq and Afghanistan have or have had PTSD or depression. Studies continue to be done to analyze the link between military service and depression, however, there are a variety of theories as to why so many service members and veterans experience depression.
The nature of service often causes a person to experience trauma. Trauma can have a lasting impact, long after a person’s experience is over. Depression can occur shortly after a person experiences trauma, or it may take years to manifest. Below are some examples of trauma that could lead a veteran to develop depression:
- Witnessing a fellow service member be injured or killed
- Experiencing an injury as the result of combat
- Experiencing an IED explosion
- Being part of a burial crew
- Living with the fear of hostile military or terrorist activity
- In-service assault or threat of assault
Female veterans are at significant risk for depression and are more than 250 percent more likely to commit suicide than their civilian counterparts. The rate of military sexual trauma female veterans face could be one of the potential reasons the rates of depression and suicide are so high among this population.
It is also important to know that veterans can still receive benefits for events that may not be linked to their service, but that occurred while they were in service. An example of this may be if a veteran’s family member passes away while they are deployed.
Direct VA Service Connection for Depression
To establish direct service connection for depression, veterans will typically need three things:
- A current diagnosis of depression—The easiest way to show proof of a diagnosis for depression is through medical records. Importantly, the diagnosis must be current.
- An in-service event or stressor—To prove an in-service event, veterans might use service treatment records, as they will have documented any injury or illness, including depression, if it was treated during active duty. Unfortunately, not all veterans have this type of evidence available to them, as many service members do not seek treatment out of fear of stigma. In this case, lay statements from the veteran and/or their family members can be particularly effective. These statements can be used to describe both the onset and progression of the veteran’s depression, as well as how it relates to service.
- A medical nexus between the depression and the in-service event—A statement from a qualified healthcare professional affirming that they believe your condition was “at least as likely as not” caused by your military service can serve as a medical nexus.

VA Ratings for Depression
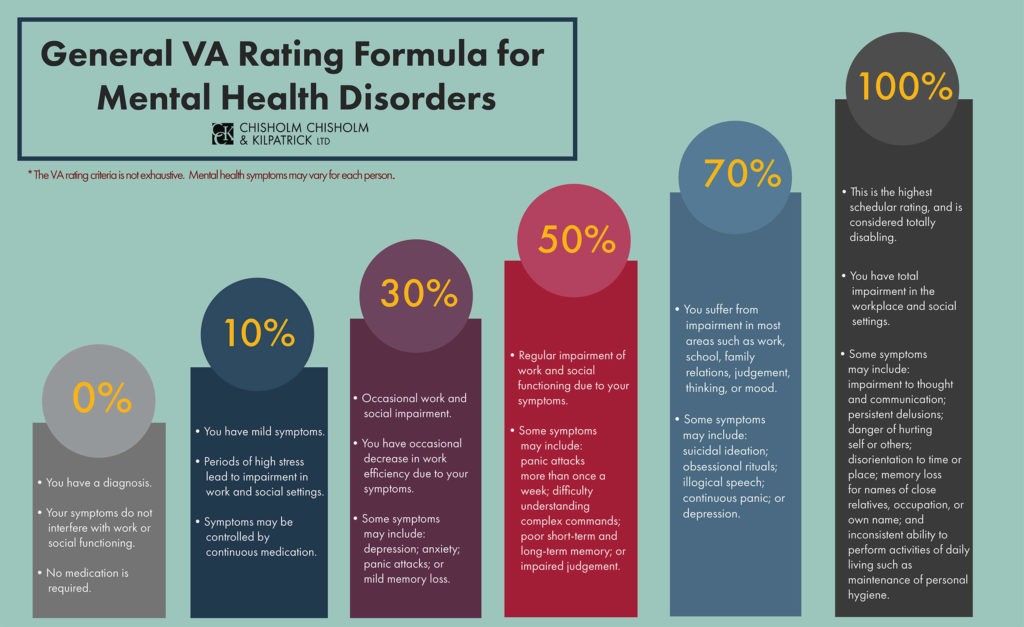
Mental health conditions can be rating anywhere from 0 percent to 100 percent. Specifically, major depressive disorder is rated under Diagnostic Code 9434. The rating given will be based on the level of social and occupational impairment a veteran experiences and the severity of symptoms.
- 100%–This rating is for veterans who experience “total occupational and social impairment.” Symptoms may include gross impairment in thought processes or communication, persistent delusions or hallucinations, grossly inappropriate behavior, persistent danger of hurting self or others, intermittent inability to perform activities of daily living (such as minimal maintenance of personal hygiene), disorientation to time or place, memory loss for names of close relatives, occupation, or name.
- 70%–Veterans rated at 70 percent experience occupational and social impairment, with deficiencies in “most” areas. Symptoms may be similar to those listed above in the 100 percent criteria. Impairment may affect the veteran’s work, school, family relations, thinking or mood. Veterans rated at this level may also experience suicidal ideation.
- 50%–The 50 percent rating is given to veterans with occupational and social impairment, specifically with “reduced reliability and productivity.” Symptoms can include panic attacks more than once a week, difficulty understanding complex commands, loss of memory, impaired judgement, disturbances of mood, and difficulty establishing and maintaining effective work and social relationships.
- 30%–To secure the 30 percent rating, veterans will experience occupational and social impairment with “occasional decrease in work efficiency” and periods of inability to perform occupational tasks. Symptoms may include depressed mood, anxiety, suspiciousness, panic attacks, chronic sleep impairment, and mild memory loss.
- 10% –10 percent ratings are given to veterans with occupational and social impairment from “mild or transient symptoms” that can decrease work efficiency or the ability to perform occupational tasks during periods of stress.
- 0%–The 0 percent rating is non-compensable, meaning that it is not associated with any financial compensation . However, this rating is still important because it establishes service connection for the condition and can potentially help the veteran receive an increased rating in the future. With the 0 percent rating, veterans have a diagnosis, but the symptoms may not be severe enough to interfere with occupational or social functioning.
Importantly, a veteran does not need to endorse all the symptoms listed in each rating criteria. A Court of Appeals for Veterans Claims case, Mauerhan v. Principi, established that the symptoms listed in Diagnostic Code 9411 (i.e., post-traumatic stress disorder) are not intended to constitute an exhaustive list, but rather serve as examples of the type and degree of the symptoms, or their effects, that would justify a particular rating.
The same case law applies when determining a disability rating for depression. Therefore, a veteran can have any number of symptoms listed in the rating criteria for depression and still meet that level of evaluation.
Secondary Service Connection and Depression
Once a veteran is service connected for depression, they may seek secondary service connection for conditions connected to their depression. Veterans may also seek secondary service connection for depression itself, as may be the case if the veteran were to develop depression as the result of a service-connected orthopedic injury.
To establish secondary service connection for a condition that stems from the veteran’s depression, the veteran will usually need:
- A current diagnosis of a condition secondary to depression
- Medical evidence showing the relationship between their depression and the secondary condition
For example, many psychotropic medications that are prescribed to treat depression can result in significant weight gain. This weight gain could then cause or exacerbate an orthopedic condition. Thus, the orthopedic condition may warrant secondary service connection.
To obtain secondary service connection for this orthopedic condition, the veteran will need a diagnosis for their orthopedic condition and medical evidence indicating that it was brought on or aggravated by their depression.
Common Conditions Secondary to Depression
Depression can be linked to a multitude of different conditions. The following list is composed of just some of the conditions which may occur as secondary to depression. Many of these conditions can also occur in the reverse order, meaning that depression could be the secondary condition.

Post-Traumatic Stress Disorder
PTSD can occur in people who have experienced or witnessed a traumatic event. Oftentimes, people with PTSD experience intrusive thoughts, avoidance, and overwhelming negative thoughts and feelings. Importantly, since all mental health conditions are evaluated using the same criteria, veterans with multiple mental health conditions (in this case PTSD and depression) will likely be assigned one combined disability rating. Similarly, veterans do not need to submit a separate claim for each mental health condition, although they are free to do so if they wish.
PTSD rating criteria is the same as depression, which is listed above. Although rated using the same criteria the diagnostic code for PTSD is 9411 while the diagnostic code for depression is typically 9434.
Migraines
Migraines are a form of headache that can bring pain, nausea, vomiting, sensitivity to light and sound, lightheadedness, and blurred vision. Sometimes an aura, which is categorized by visual disturbances such as flashes of light, may come before a migraine. Migraine triggers are thought to include hormonal imbalance, alcohol, stress, sensory stimulation, certain foods, and changes in environment.
Research into the relationship between migraines and depression has indicated that people who experience migraines are five times more likely to develop depression than those who do not experience migraines. Migraines are a chronic condition and can often cause a significant amount of recurring pain. Experiencing migraines routinely can cause a person to feel angry, sad, or defeated and may lead to depression.
Conversely, people who have depression may begin to experience migraines. In this case, the depression is not a response to the migraines, but rather the migraines occur as a symptom of depression. This can happen after a person has been living with depression for some time. Anxiety caused by migraines, such as worrying about when the next migraine attack may occur, can also exacerbate depression and its symptoms.
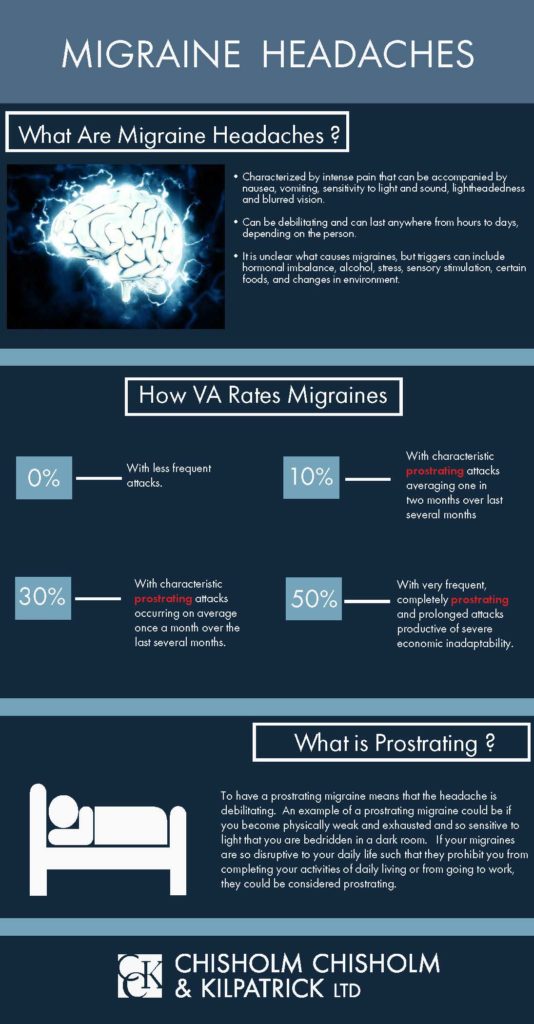
VA will rate migraine headaches using 38 C.F.R. 4.124a. Migraines are specifically rated under Diagnostic Code 8100. This diagnostic code includes ratings from 0 to 50 percent, with each rating depending on the severity and frequency of migraines.
Rating criteria is listed below:
- 50%–This rating is given to veterans who experience frequent prostrating and prolonged attacks productive of severe economic inadaptability.
- 30%–Veterans experience characteristic prostrating attacks occurring on average of once a month over the last several months.
- 10%–To receive the 10 percent rating, the veteran will generally experience characteristic prostrating attacks averaging one in two months over the past several months.
- 0%–Veterans who receive service connection, but a 0 percent rating generally experience less frequent attacks.
Importantly, though VA uses the term “prostrating” to describe migraines and the establish severity, there is no VA regulation that specifically defines “prostrating.” However, generally speaking, “prostrating” means that the veteran’s migraine headaches are so severe and debilitating that they are required to lay down for an extended period of time due to complete exhaustion and physical weakness. Typically, prostrating migraines also require veterans to stop all activity and possibly take medication or seek medical attention.
Anxiety
Anxiety is defined as intense, excessive, and persistent worry and fear about everyday situations. Symptoms can include restlessness, excessive worrying, difficulty concentrating, rapid heartbeat, twitching or trembling, muscle tension, difficulty breathing, and nausea.
Importantly, in-service causes of depression and anxiety do not have to be due to a military activity. Rather, the cause merely needs to have happened during service. Oftentimes veterans are experiencing problems not directly related to the military that still affect their functioning during service. For example, if a veteran is deployed to another country and they are experiencing problems with their family at home, they might become depressed and anxious over their inability to be with their family while stationed abroad. Again, as long as the factors causing the veteran’s symptomatology, or the symptomatology itself, manifested during service, the veteran is eligible for service connection.
Like with PTSD, anxiety is also rated as a mental health condition. This means that veterans will receive one combined rating for all their mental health conditions, instead of two separate ratings.
Sleep Apnea
There are three main types of sleep apnea:
- Obstructive Sleep Apnea – the most common form of sleep apnea; occurs when the throat muscles intermittently relax and block your airway during sleep
- Central Sleep Apnea – occurs when your brain doesn’t send proper signals to the muscles that control breathing
- Complex (Mixed) Sleep Apnea Syndrome – occurs when someone has both obstructive sleep apnea and central sleep apnea
Sleep apnea can cause a myriad of symptoms, such as snoring, gasping for air, dry mouth, headaches, insomnia, excessive daytime sleepiness, and difficulty concentrating.
As sleep apnea can affect a person’s sleep schedule, many people who experience sleep apnea can also experience depression. Patients with sleep apnea also suffer a lack of oxygen, which may cause changes to the brain and can cause depression. Similarly, sleep apnea may cause inflammation in the body and affect neurotransmitter activity, which could then contribute to symptoms of depression.
Sleep apnea is rated under 38 CFR § 4.97, Diagnostic Code 6847 – Sleep Apnea Syndromes (obstructive, central, mixed). Veterans are assigned a 0, 30, 50, or 100 percent rating depending on the severity of their condition. The rating criteria are as follows:
- 100% – chronic respiratory failure with carbon dioxide retention, the need for a tracheostomy, or cor pulmonale (i.e., the enlargement or failure of the right side of the heart due to lung disease)
- 50% – if a veteran requires the use of a breathing assistance device, such as a CPAP machine
- 30% – the veteran is experiencing persistent daytime hypersomnolence (i.e., a condition characterized by chronic daytime sleepiness that does not improve even with sufficient sleep)
- 0% – if the veteran’s condition is asymptomatic (i.e., condition that is not producing symptoms) but has a documented sleep disorder
Restless Leg Syndrome
Restless leg syndrome, or Willis-Ekbom Disease, is a condition that can cause painful and uncomfortable leg sensations in the legs as well as the irresistible urge to move them. These sensations can occur most commonly in the late afternoon or evening and can become particularly excruciating at night. The nature of RLS can make it difficult to sleep at night, whether it be falling asleep or returning to sleep once having been awoken.
As RLS can cause consistent pain and can disturb a person’s sleep schedule, it can also cause a person to become depressed.
VA rates restless leg syndrome under Diagnostic Code 8620, which relates to neuritis. The ratings may also range from mild to severe:
- Mild – 10%
- Moderate – 20%
- Moderately Severe – 40%
- Severe – 60%
Erectile Dysfunction
Erectile dysfunction is a condition that can stand in the way of a happy, fulfilling life. As such, many who experience the condition develop depression as a result.
There is no specific disability rating for erectile dysfunction. Instead, VA rates the condition under 38 C.F.R. § 4.115b. Examples of erectile dysfunction related listings include:
- Code 7520: If doctors removed half or more than half of your penis, you receive a rating of 30 percent.
- Code 7521: If doctors removed your glans, your rating is 20 percent.
- Code 7522: If your penis cannot become erect because of a physical deformity, you receive a 20-percent rating.
- Code 7523: If your erectile dysfunction is due to atrophied testicles, a condition often resulting in reduced testosterone and thus a lower sex drive, you receive a 20-percent rating if the condition affects both testicles, and a 0 percent rating if it affects only one testicle.
- Code 7524: If you had both testicles removed due to a service-connected event, you receive a 30-percent rating; if you had one testicle removed due to a service-connected event, you receive a 0-percent rating.
Generally, VA will grant a 0-percent rating for erectile dysfunction unless you are eligible under the diagnostic codes above. However, service connection for erectile dysfunction, even at 0 percent, makes veterans eligible for Special Monthly Compensation (SMC) for loss of use of a creative organ. This is known as SMC (k) and it is paid out in your monthly VA compensation check.
Gastrointestinal Conditions
As part of the brain-gut connection, some gastrointestinal conditions may arise when a person has depression. Some of these gastrointestinal conditions can include GERD (gastro-esophageal reflux disease), irritable bowel disease, and ulcerative colitis.
Some veterans may be eligible for presumptive service connection for their gastrointestinal condition, depending on certain factors. For example, former prisoners of war (POWs) who were captive for 30 days or more can receive presumptive service connection for certain gastrointestinal conditions. Additionally, veterans who served at Camp Lejeune for 30 days or more may be eligible for presumptive service connection for liver cancer, a gastrointestinal condition.
VA rates gastrointestinal diseases under 38 CFR § 4.114, Schedule of Ratings for the Digestive System. There are multiple diagnostic codes for the various gastrointestinal conditions that fall under this rating schedule. VA will compare your symptomatology to that which is listed in the rating criteria in order to assign a disability evaluation. It is helpful to look up the diagnostic code that corresponds to your condition to determine what VA is looking for during the rating process.
Seizures
Some veterans with severe depression may experience seizures. Additionally, seizures are a common side effect of traumatic brain injury, which can also cause depression. As such, many veterans with depression or TBI also experience seizures.
There are a few ways that VA rates seizures, depending on the type of seizure it is. Some are classified as major seizures, while others are classified as minor.
Examples include, but are not limited to, the following:
- Grand mal epilepsy (DC 8910): Features a loss of consciousness and violent muscle contractions.
- Petit mal epilepsy or absence seizures (DC 8911): Involves brief and sudden lapses of consciousness.
- Focal motor epilepsy (DC 8912): Appears to be the result of abnormal activity in just one area of the brain. Two types of focal motor epilepsy include focal seizures without loss of consciousness and focal dyscognitive seizures.
- Jacksonian epilepsy (DC 8912): Involves a brief alteration in movement, sensation, or nerve.
- Psychomotor epilepsy (DC 8914): Occurs in the temporal lobe of the brain and results in the impairment of responsiveness and awareness.
Although each type of epilepsy or seizure condition has its own diagnostic code (DC), they are all still evaluated under the general rating formula outlined below.
| Rating Percentage | Major Seizures | Minor Seizures |
| 100% | 12 or more in the past year | N/A |
| 80% | 4-11 in the past year | 11 or more per week |
| 60% | 3 in the past year | 9-10 per week |
| 40% | 2 in the past year | 5-8 per week |
| 20% | 1 in the past 2 years | 2 in the past 6 months |
| 10% | Requires constant medication to control seizures or there is a definite diagnosis of epilepsy with history of seizures | Requires constant medication to control seizures or there is a definite diagnosis of epilepsy with history of seizures |
Liver Conditions
Liver conditions can be linked to depression in several ways. Veterans who were exposed to the contaminated waters at Camp Lejeune may have developed liver cancer, which can contribute to depression. Additionally, a depressed veteran may turn to alcohol as a coping mechanism, which can cause significant damage to the liver. Veterans cannot be directly service-connected for alcoholism; however, they can be service-connected on a secondary basis for conditions that arise from alcoholism, if the alcoholism is due to a service-connected condition.
As such, veterans can receive benefits if, as a result of this prolonged alcohol use, they develop cirrhosis of the liver. Alcoholism may also serve as the as a bridge to connect a veteran’s primary service-connected condition to the secondary condition they developed as a result of their alcoholism. For example, alcoholism can serve as an intermediate step between a veteran’s service-connected depression and secondary service-connected liver condition.
VA rates cirrhosis of the liver under Diagnostic Code 7312. The rating criteria is listed below:
- 100%– Symptoms include generalized weakness, substantial weight loss, and persistent jaundice, or; with one of the following refractory to treatment: ascites, hepatic encephalopathy, hemorrhage from varices or portal gastropathy (erosive gastritis)
- 70%–History of two or more episodes of ascites, hepatic encephalopathy, or hemorrhage from varices or portal gastropathy (erosive gastritis), but with periods of remission between attacks
- 50%–History of one episode of ascites, hepatic encephalopathy, or hemorrhage from varices or portal gastropathy (erosive gastritis)
- 30%–Portal hypertension and splenomegaly, with weakness, anorexia, abdominal pain, malaise, and at least minor weight loss
- 10%–Symptoms such as weakness, anorexia, abdominal pain, and malaise
Additionally, in order to receive a rating under this diagnostic code, abnormal liver function tests and documentation of cirrhosis, through a biopsy or imaging, must be submitted.
Orthopedic Conditions
Oftentimes, orthopedic conditions severely impact a person’s mobility. This can lead to depression, as a person with an orthopedic condition may not be able to participate in the activities they used to enjoy or live their day-to-day life. If a veteran develops depression because of their orthopedic condition, they can receive secondary service connection for their depression.
Orthopedic conditions are rated under a variety of diagnostic codes, depending on the condition. Typically, range of motion will be used to assess an orthopedic condition and assign a disability rating.

Tinnitus
Tinnitus is a condition that causes a person to experience a persistent ringing sensation in their ears. Tinnitus is one of the most common conditions for which veterans become service-connected. Exposure to loud noises, such as gunfire, aircrafts, heavy machinery, and other noises associated with military service, can cause tinnitus. Additionally, traumatic brain injury, which can occur as the result of any blow to the head, can also cause tinnitus. Tinnitus can make disturb a person’s sleep schedule, and as a result, cause depression. A 2015 study found that in a sample of veterans who were diagnosed with tinnitus, about 58 percent also had depression.
VA rates tinnitus under 38 CFR § 4.87, Schedule of Ratings – Ear, Diagnostic Code 6260. Most veterans are assigned a 10 percent rating for tinnitus, which takes into account both ears.
Insomnia
Insomnia is a sleep disorder marked by difficulty falling asleep or staying asleep, even when a person has the chance to do so. The two main types of insomnia are acute (short-term) and chronic (long-term).
- Acute Insomnia—This form usually only lasts for a short period of time, likely less than one month.
- Chronic Insomnia—Chronic insomnia is more complex than acute insomnia and occurs several times per week. This form can last at least one month or longer.
Depression, as well as anxiety and PTSD, can cause insomnia. Insomnia can also cause depression, meaning that secondary service connection can be established either way. However, in order to receive benefits for insomnia, VA will require the veteran to undergo a sleep study.
VA will typically rate insomnia according to the Schedule of Ratings for Mental Disorders (38 CFR § 4.130). However, VA tends to rate the condition as a component of an underlying mental health condition, such as depression.
For example, if a veteran is service connected for depression and suffers from insomnia as a result, it is likely that VA will consider the sleep condition in its overall evaluation of the veteran’s depression.
Ratings for insomnia itself can range from 0 to 100 percent. Below are the criteria for each rating:
- 100%—Presents total occupational and social impairment
- 70%— Occupational and social impairment, with deficiencies in most areas
- 50%—Presents occupational/social impairment with reduced reliability
- 30% Occupational and social impairment with occasional decrease in work efficiency and intermittent periods of inability to perform occupational tasks
- 10%—Occupational or social impairment due to mild or transient symptoms
- 0%—If diagnosed but symptoms are not severe enough to interfere in occupational or social settings
- Although 0% ratings often do not result in compensation, they are still important because VA recognizes service connection.
Conditions Caused by Anti-Depressants
Some of the above conditions may be related directly to depression, while others, like seizures or gastrointestinal conditions, can be side effects of medications like anti-depressants. Veterans who develop conditions as a result of their depression medication are eligible for secondary service connection for those conditions.
VA Compensation and Pension (C&P) Exams for Secondary Conditions
The process for obtaining secondary service connection for conditions related to depression is comparable to that for direct service connection. This means that a compensation and pension exam (C&P) may be requested.
The C&P exam will be performed by a VA examiner or a VA-contracted examiner. They may physically examine the veteran, if applicable, or interview the veteran regarding the secondary condition. Since the condition is secondary to depression, the examiner may ask questions regarding the veteran’s mental health.
It is important to attend any C&P exams that VA requests, even if they request two exams: one for depression and one for the secondary condition. Though the exams may seem redundant, it is crucial that the veteran attends because VA may deny the claim if they do not. If the veteran must miss a C&P exam, they should contact VA as soon as possible to try to reschedule.
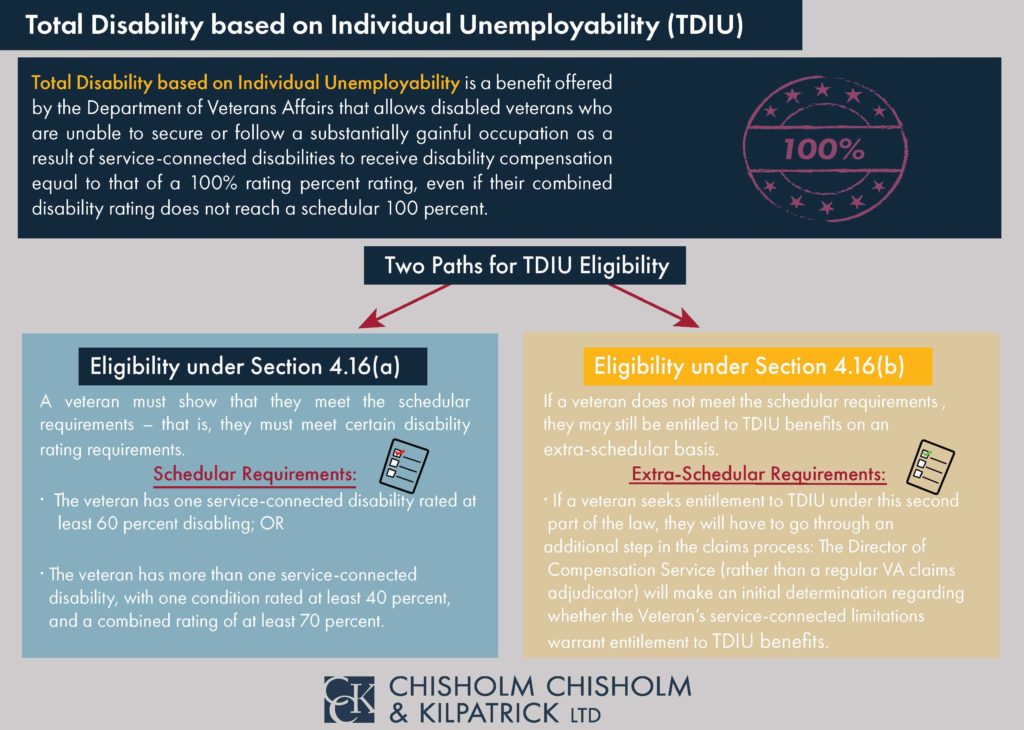
TDIU and Conditions Secondary to Depression
Secondary conditions can be very beneficial to help boost a veteran’s overall combined rating. Overall combined ratings can help a veteran achieve TDIU.
TDIU, or total disability based on individual unemployability, is a monthly VA benefit that compensates veterans at the 100 percent level if they are prevented from working because of their condition(s).
In order to be eligible for schedular TDIU, veterans must have one condition rated at 60 percent minimum OR two conditions that can be combined to reach 70 percent, where one condition is at minimum 40 percent. As such, secondary service connection can be extremely helpful in boosting veterans to the 70 percent minimum needed for multiple conditions to achieve TDIU. The criteria for schedular TDIU is outlined under 38 CFR § 4.16a.
Veterans who do not meet the necessary criteria for schedular TDIU may be eligible for extraschedular TDIU. For this form of TDIU, veterans must prove that their condition(s) uniquely hinder their ability to maintain substantially gainful employment. Extraschedular TDIU is rated under 38 CFR § 4.16b.
Resources for Veterans Experiencing a Mental Health Crisis
Veterans who experience depression, or have conditions stemming from their depression, may experience a mental health crisis or contemplate suicide. Importantly, veterans should know that help is available, and they do not need to be alone if they are experiencing such a crisis.
The Veteran’s Crisis Hotline offers 24/7 assistance. It is confidential and anonymous, so veterans do not need to fear any stigma or retaliation for reaching out. This resource is available to veterans, even if they do not have VA health care or have not been service-connected for any VA benefits. The service is toll-free and veterans, as well as their family members and friends, can speak with a qualified, caring VA responder. Veterans may call the hotline at 1-800-273-8255 and press 1, or text 838255.
Veterans can also utilize a confidential online chat session at VeteransCrisisLine.net/Chat. Additionally, this site offers a self-check quiz for veterans to learn more about whether stress and depression may be affecting them.
To learn more about other resources available for veterans experiencing a mental health crisis, and what VA has done to respond to the veterans’ suicide epidemic, you can read our blog: What is VA Doing to Help the Veterans’ Suicide Epidemic.
Need Help with Your VA Disability Benefits for a Condition Secondary to Depression?
Claims for conditions secondary to depression can be complicated due to the nature of depression. Specifically, the stigma of mental health conditions may have prevented veterans from seeking treatment while still in service and, as such, a lack of in-service evidence may be an obstacle in the way of service connection for depression or secondary service connection.
If your claim for service connection for depression, or secondary service connection for a condition caused by your depression, has been denied, Chisholm Chisholm & Kilpatrick may be able to help. Our team has helped veterans with their appeals for service connection for depression, increased ratings for depression, and conditions secondary to depression. Contact us today for a free case review at 800-544-9144.
About the Author
Share this Post