VA Disability Benefits for Sleep Disorders Secondary to Depression
CCK Law: Our Vital Role in Veterans Law
What is Depression?
Depression, or major depressive disorder, is a serious medical condition that can interfere with necessary activities of life, such as eating, sleeping, and working. Depression can affect how a person feels and thinks. As such, depression often takes a significant mental, emotional, and physical toll on a person.
Symptoms of Depression
- Feelings of sadness, fatigue, worthlessness, guilt, or hopelessness
- Loss of interest or pleasure in usual activities
- Disturbances in sleep
- Anxiety or restlessness
- Irritability
- Difficulty concentrating or remembering things
- Loss of appetite and weight loss or increased appetite and weight gain
- Thoughts of death or suicide
How Common is Depression in Veterans?
Depression is very common among servicemembers and veterans. A 2014 study found that nearly 1 in 4 active duty servicemembers showed signs of a mental health condition.
The Substance Abuse and Mental Health Services Administration also determined that approximately 18.5 percent of veterans returning from Iraq and Afghanistan have or have had PTSD or depression. Studies continue to be done to analyze the link between military service and depression, however, there are a variety of theories as to why so many service members and veterans experience the condition.
Why is Depression So Prevalent Among Veterans?
The nature of service can cause trauma which can have a lasting impact, long after a person’s experience is over. Depression can occur shortly after a person experiences trauma, or it may take years to manifest. Below are some examples of trauma that could lead a veteran to develop depression:
- Witnessing a fellow service member be injured or killed
- Experiencing an injury as the result of combat
- Experiencing an IED explosion
- Being part of a burial crew
- Living with the fear of hostile military or terrorist activity
- In-service assault or threat of assault
Female veterans are at significant risk for depression and are more than 250 percent more likely to commit suicide than their civilian counterparts. The rate of military sexual trauma female veterans face could be one of the potential reasons the rates of depression and suicide are so high among this population.
What Are Sleep Disorders Secondary to Depression?
As one of the symptoms of depression can be disturbances in sleep, many veterans may experience sleep disorders as a result of their depression.
Some sleep disorders that can be related to depression can include:
Sleep Apnea
Sleep apnea is sleep disorder that affects a person’s breathing during the course of the night. Generally, there are three types of sleep apnea:
- Obstructive Sleep Apnea – the most common form of sleep apnea; occurs when the throat muscles intermittently relax and block your airway during sleep
- Central Sleep Apnea –occurs when your brain does not send the proper signals to the muscles that control breathing
- Complex (Mixed) Sleep Apnea Syndrome –occurs when someone has both obstructive sleep apnea and central sleep apnea
People with sleep apnea may experience loud snoring, gasping for air during the night, excessive daytime sleepiness, dry mouth, and difficulty concentrating.
Insomnia
Insomnia is a sleep disorder marked by difficulty falling asleep or staying asleep, even when a person has the chance to do so. People with the condition can feel dissatisfied with their sleep and experience negative outcomes related to their energy level, mood, health, work performance, and quality of life.
The two main types of insomnia are acute (short-term) and chronic (long-term).
- Acute Insomnia—This form usually only lasts for a short period of time, likely less than one month.
- Chronic Insomnia—Chronic insomnia is more complex than acute insomnia and occurs several times per week. This form can last at least one month or longer.
Narcolepsy
Narcolepsy is a chronic sleep disorder characterized by overwhelming hypersomnolence (i.e., daytime drowsiness) and sudden attacks of sleep. Individuals with this condition often find it difficult to stay awake for prolonged periods of time, regardless of the circumstances (e.g., time of day, engagement in activities, amount of sleep obtained the night before). As a result, narcolepsy can cause significant disruptions and impairments in a person’s daily routine. There are two types of narcolepsy:
- Type 1 narcolepsy – occurs with cataplexy (i.e., sudden loss of muscle tone); can be triggered by strong emotion
- Type 2 narcolepsy – occurs without cataplexy
Symptoms of narcolepsy can include daytime sleepiness, sleep paralysis, and hallucinations. While depression may not necessarily cause narcolepsy, many people who have narcolepsy also experience depression. Additionally, a study published in 2018 noted that more than 50 percent of patients who were studied that had narcolepsy and comorbid depression had been diagnosed with depression prior to narcolepsy. While there is not enough evidence to make any definitive link about depression causing narcolepsy, it is clear that depression and narcolepsy do share some symptomology.
Establishing Direct Service Connection for Depression
To file a claim for VA disability benefits for depression, veterans will first need to become service connected. When seeking service connection, veterans will generally need to submit the following to VA:
- A current diagnosis of depression—The easiest way to show proof of a diagnosis for depression is through medical records. Importantly, the diagnosis must be current.
- An in-service event or stressor—To prove an in-service event, veterans might use service treatment records, as they will have documented any injury or illness, including depression, if it was treated during active duty. Unfortunately, not all veterans have this type of evidence available to them, as many service members do not seek treatment out of fear of stigma. In this case, lay statements from the veteran and/or their family members can be particularly effective, as they can describe both the onset and progression of the veteran’s depression, as well as how it relates to service.
- A medical nexus between the depression and the in-service event—A statement from a qualified healthcare professional affirming that they believe your condition was “at least as likely as not” caused by your military service can serve as a medical nexus.

Veterans can submit their claim using VA Form 21-526EZ. The form can be submitted to VA in the following ways:
- Online – using VA’s eBenefits platform
- By mail – directed to the Department of Veterans Affairs, Evidence Intake Center, PO Box 4444 in Janesville, WI 53547-4444
- In person – bringing a completed VA Form 21-526EZ to a VA Regional Office near you
- With a legal representative – completing the form with a Veterans Service Organization (VSO) or a VA accredited agent or attorney
Establishing Secondary Service Connection for a Sleep Disorder
Once the veteran has been service connected for depression, they may wish to file a claim for secondary service connection for their sleep disorder. Filing a claim for secondary service connection is much like filing a claim for direct service connection. Veterans can use the same form, VA 21-526EZ, to file for secondary service connection for sleep disorders secondary to depression.
When submitting a claim for secondary service connection, the veteran should submit:
- A current diagnosis of a sleep disorder secondary to depression
- Medical evidence showing the relationship between their depression and the sleep disorder
VA Ratings for Depression
Mental health conditions can be rated from 0 percent to 100 percent. Specifically, major depressive disorder is rated under Diagnostic Code 9434. The rating given will be based on the level of social and occupational impairment a veteran experiences and the severity of symptoms.
- 100%–This rating is for veterans who experience “total occupational and social impairment.” Symptoms may include gross impairment in thought processes or communication, persistent delusions or hallucinations, grossly inappropriate behavior, persistent danger of hurting self or others, intermittent inability to perform activities of daily living (such as minimal maintenance of personal hygiene), disorientation to time or place, memory loss for names of close relatives, occupation, or name.
- 70%–Veterans rated at 70 percent experience occupational and social impairment, with deficiencies in “most” areas. Symptoms may be similar to those listed above in the 100 percent criteria. Impairment may affect the veteran’s work, school, family relations, thinking or mood. Veterans rated at this level may also experience suicidal ideation.
- 50%–The 50 percent rating is given to veterans with occupational and social impairment, specifically with “reduced reliability and productivity.” Symptoms can include panic attacks more than once a week, difficulty understanding complex commands, loss of memory, impaired judgement, disturbances of mood, and difficulty establishing and maintaining effective work and social relationships.
- 30%–To secure the 30 percent rating, veterans will experience occupational and social impairment with “occasional decrease in work efficiency” and periods of inability to perform occupational tasks. Symptoms may include depressed mood, anxiety, suspiciousness, panic attacks, chronic sleep impairment, and mild memory loss.
- 10%–10 percent ratings are given to veterans with occupational and social impairment from “mild or transient symptoms” that can decrease work efficiency or the ability to perform occupational tasks during periods of stress.
- 0%–The 0 percent rating is non-compensable, meaning that it is not associated with any financial compensation. However, this rating is still important because it establishes service connection for the condition and can potentially help the veteran receive an increased rating in the future. With the 0 percent rating, veterans have a diagnosis, but the symptoms may not be severe enough to interfere with occupational or social functioning.
Importantly, a veteran does not need to demonstrate all the symptoms listed in each rating criteria. A Court of Appeals for Veterans Claims case, Mauerhan v. Principi, established that the symptoms listed in Diagnostic Code 9411 (i.e., post-traumatic stress disorder) are not intended to constitute an exhaustive list, but rather serve as examples of the type and degree of the symptoms, or their effects, that would justify a particular rating. The same case law applies when determining a disability rating for depression. Therefore, a veteran can have any number of symptoms listed in the rating criteria for depression and still meet that level of evaluation.
VA Ratings for Sleep Disorders
Sleep disorders are rated under varying diagnostic codes, depending on the disorder. Ratings are also determined by the disorder.
Sleep Apnea
VA rates sleep apnea under 38 CFR § 4.97, Diagnostic Code 6847. Veterans are assigned either a 0, 30, 50, or 100 percent rating depending on the severity of their condition.
- 0%–This rating is non-compensable, meaning that there is no compensation associated with the rating, however it does establish service connection. The rating is given to veterans who have a diagnosis of sleep apnea, but do not experience any symptoms.
- 30%–The 30 percent rating is awarded to veterans who experience chronic daytime sleepiness as the result of their sleep apnea, or hypersomnolence.
- 50%–The 50 percent rating is given to veterans who require the use of a CPAP machine. This rating is often the most common, since many people with sleep apnea require a CPAP machine.
- 100%–Veterans who receive the 100 percent rating are considered totally disabled. Veterans with the 100 percent rating may experience chronic respiratory failure with carbon dioxide retention or cor pulmonale, or; requires tracheostomy.
Insomnia
VA will rates insomnia using the Schedule of Ratings for Mental Disorders (38 CFR § 4.130). However, VA tends to rate the condition as a component of an underlying mental health condition.
With depression, VA will consider insomnia in the overall evaluation for depression, rather than assigning two separate ratings for insomnia and depression. Assigning two ratings for conditions with the same symptoms is considered pyramiding.
As such, if a veteran has a psych condition and insomnia, they will only get one rating, not two. If the veteran’s insomnia is not caused by a mental health condition, but some other condition (e.g., orthopedic condition), then VA will likely assign a separate disability rating for insomnia based on the Schedule of Ratings for Mental Disorders:
- 100%—Presents total occupational and social impairment
- 70%— Occupational and social impairment, with deficiencies in most areas
- 50%—Presents occupational/social impairment with reduced reliability
- 30% Occupational and social impairment with occasional decrease in work efficiency and intermittent periods of inability to perform occupational tasks
- 10%—Occupational or social impairment due to mild or transient symptoms
- 0%—If diagnosed but symptoms are not severe enough to interfere in occupational or social settings
Narcolepsy
Settings VA rates narcolepsy according to 38 CFR § 4.124a, Schedule of Ratings – Neurological Conditions and Convulsive Disorders, Diagnostic Code 8911 (i.e., epilepsy, petit mal). Since narcolepsy can severely impact your ability to live a normal life, VA rates it on the same scale as a minor seizure disorder. The rating criteria are as follows:
- 100% – averaging at least one major seizure per month over the last year
- 80% – averaging at least one major seizure in 3 months over the last year; or more than 10 minor seizures weekly
- 60% – averaging at least one major seizure in 3 months over the last year; or more than 10 minor seizures weekly
- 40% – at least one major seizure in 6 months or 2 in the last year; or averaging at least 5 to 8 minor seizures weekly
- 20%- at least one major seizure in the last 2 years; or at least 2 minor seizures in the last 6 months
- 10% – a confirmed diagnosis of epilepsy with a history of seizures
Importantly, when continuous medication is shown necessary for the control of epilepsy, the minimum evaluation will be 10 percent; however, this rating will not be combined with any other rating for epilepsy. Furthermore, if the veteran experiences both major and minor seizures, VA adjudicators should rate the predominating type.
Compensation and Pension Exams for Sleep Disorders and Depression
During the claims and appeals process, VA may request a compensation and pension exam (C&P). C&P exams are performed by a VA examiner or a VA-contracted examiner. They may physically examine the veteran, if applicable, or interview the veteran regarding the secondary condition. With sleep disorders secondary to depression, the examiner may ask questions regarding the veteran’s mental health. A sleep study will likely be required as well.
It is important to attend any C&P exams that VA requests, even if they request two exams: one for depression and one for the sleep disorder. Though the exams may seem redundant, it is crucial that the veteran attends because VA may deny the claim if they do not. If the veteran must miss a C&P exam, they should contact VA as soon as possible to try to reschedule.
TDIU With Sleep Disorders and Depression
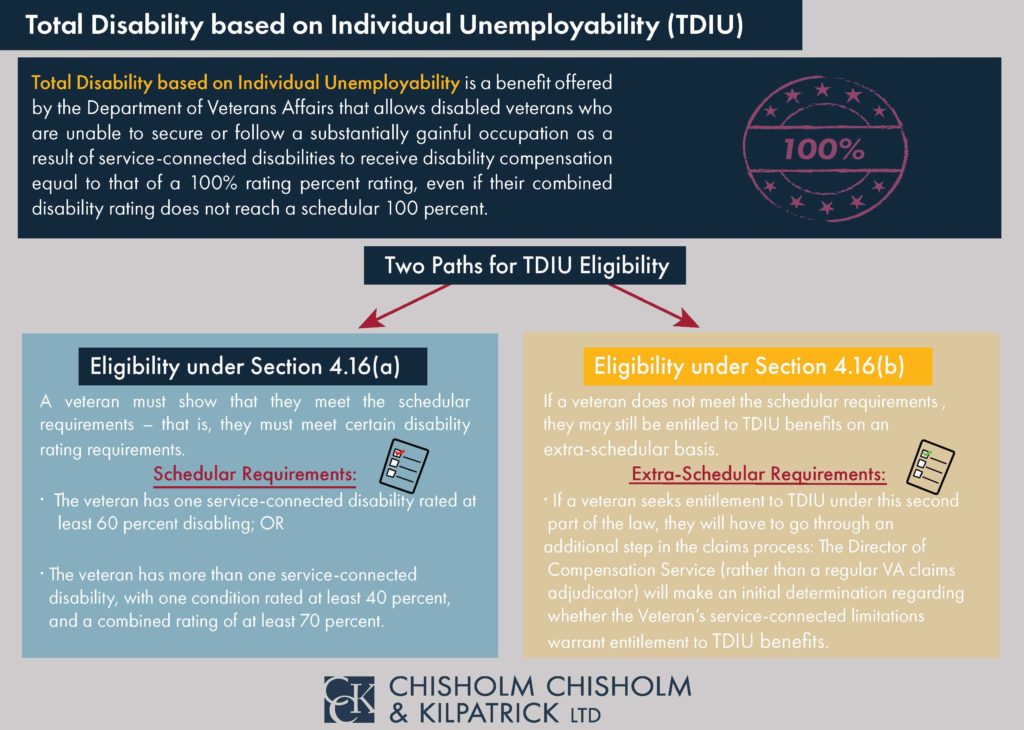
Sleep disorders secondary to depression have the potential to make a veteran eligible for TDIU where the veteran otherwise may not be eligible. Specifically, these secondary ratings can help boost a veteran’s overall combined rating to achieve TDIU.
TDIU, or total disability based on individual unemployability, is a monthly VA benefit that compensates veterans at the 100 percent level if they are prevented from working because of their conditions.
In order to be eligible for Schedular TDIU, veterans must have one condition rated at 60 percent minimum OR two conditions that can be combined to reach 70 percent, where one condition is at minimum 40 percent. As such, secondary service connection can be extremely helpful in boosting veterans to the 70 percent minimum needed for multiple conditions to achieve TDIU. The criteria for schedular TDIU is outlined under 38 CFR § 4.16a.
Veterans who do not meet the necessary criteria for schedular TDIU may be eligible for extraschedular TDIU. For this form of TDIU, veterans must prove that their conditions uniquely hinder their ability to maintain substantially gainful employment. Extraschedular TDIU is rated under 38 CFR § 4.16b.
Resources for Veterans Experiencing a Mental Health Crisis
Depression is a serious mental health condition, meaning that many veterans with this condition may experience a mental health crisis or contemplate suicide.
Importantly, veterans should know that help is available if they are experiencing such a crisis.
The Veteran’s Crisis Hotline offers 24/7 assistance. It is confidential and anonymous, so veterans do not need to fear any stigma or retaliation for reaching out. This resource is available to veterans, even if they do not have VA health care or have not been service-connected for any VA benefits. The service is toll-free and veterans, as well as their family members and friends, can speak with a qualified, caring VA responder. Veterans may call the hotline at 1-800-273-8255 and press 1, or text 838255.
Veterans can also utilize a confidential online chat session at VeteransCrisisLine.net/Chat. Additionally, veterans may search the website to find local resources and learn more about the effects of depression.
Need Help with Your VA Disability Benefits for a Sleep Disorder Secondary to Depression?
Getting benefits for sleep disorders secondary to depression can be challenging, especially if you lack the in-service evidence to secure your initial service-connected depression.
If your claim for service connection for depression, or secondary service connection for a sleep disorder caused by your depression, has been denied, Chisholm Chisholm & Kilpatrick may be able to help. Our team has helped veterans navigate the appeals process and we may be able to help you. Contact us today for a free case review.
About the Author
Share this Post
