PTSD Secondary Conditions and VA Ratings
What is Post-Traumatic Stress Disorder (PTSD)?
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that occurs as a result of experiencing a distressing, shocking, or otherwise traumatic event. Many veterans develop PTSD from events they witnessed or experienced during their military service.
PTSD can be diagnosed by a medical professional, whether it be a therapist, psychiatrist, or general practitioner.
Symptoms of PTSD
- Intrusive Thoughts or Memories
- Flashbacks
- Avoidance of Certain Situations, People, or Places
- Overwhelmingly Negative Thoughts or Feelings
- Irritability or Angry Outbursts
- Anxiety
- Depression
- Loss of interest in activities or feelings of numbness
- Difficulty sleeping
- Intense nightmares
- Trouble concentrating
- Easily startled
Importantly, symptoms of PTSD can manifest differently from person to person. The severity of symptoms can also vary.
What is Secondary Service Connection?
A secondary service-connected condition is one that resulted from a separate condition that is already service-connected. Veterans can receive disability benefits for secondary service-connected disabilities, just the same way they receive benefits for primary service-connected disabilities. To become secondarily service-connected, the veteran will usually need to prove that their condition developed or was aggravated by an already service-connected condition.
- Aggravation—VA will compensate veterans for medical conditions that existed at the time of entry into service that were made worse or “aggravated” by service. However, the burden falls on the veteran to establish aggravation. VA will then need to determine whether the veteran has shown an increase in disability during their service.
Common Secondary Conditions to PTSD
With PTSD, several different conditions could arise as the result of post-traumatic stress disorder. Below are some of the most common examples:
Sleep Apnea Secondary to PTSD
- Sleep Apnea—Sleep apnea is a potentially serious sleep disorder in which a person’s breathing is repeatedly interrupted during the course of the night.
There are three main types of sleep apnea:
- Obstructive Sleep Apnea–This is the most common form of sleep apnea. It occurs when the throat muscles intermittently relax and block your airway during sleep.
- Central Sleep Apnea–This form of sleep apnea occurs when your brain doesn’t send proper signals to the muscles that control breathing.
- Complex (Mixed) Sleep Apnea–– Complex, or mixed, sleep apnea occurs when someone has both obstructive sleep apnea and central sleep apnea
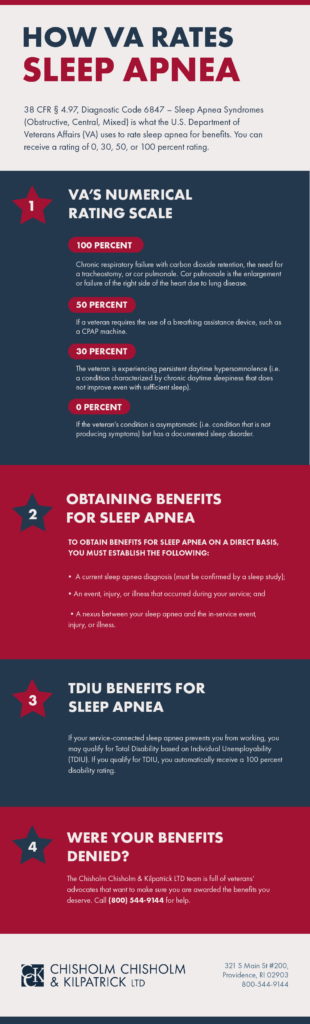
To confirm a sleep apnea diagnosis for VA disability compensation purposes, VA requires that a sleep study be conducted. The ratings for sleep apnea are as follows:
- “100% – chronic respiratory failure with carbon dioxide retention, the need for a tracheostomy, or cor pulmonale. Cor pulmonale is the enlargement or failure of the right side of the heart due to lung disease.
- 50% – if a veteran requires the use of a breathing assistance device, such as a CPAP machine
- 30% – the veteran is experiencing persistent daytime hypersomnolence (i.e., a condition characterized by chronic daytime sleepiness that does not improve even with sufficient sleep)
- 0% – if the veteran’s condition is asymptomatic (i.e., condition that is not producing symptoms) but has a documented sleep disorder”
Research has indicated that veterans with PTSD are at a higher risk of developing sleep apnea. There is also a direct correlation regarding the severity of the two conditions, meaning the more severe a veteran’s PTSD is, the more severe their sleep apnea will be.
The correlation between the two conditions is partly because many factors that can aggravate PTSD can also exacerbate sleep apnea. For example, sleep deprivation, insomnia, hyperarousal, and daytime sleepiness can all affect both PTSD and sleep apnea.
Depression Secondary to PTSD
Depression—Depression is a serious mental health condition that affects the way a person thinks, feels, and acts. Symptoms can manifest differently amongst individuals, but a person with depression may experience persistent feelings of sadness or hopelessness, lack of motivation, difficulty sleeping, change in appetite, irritability, fatigue, or suicidal thoughts.
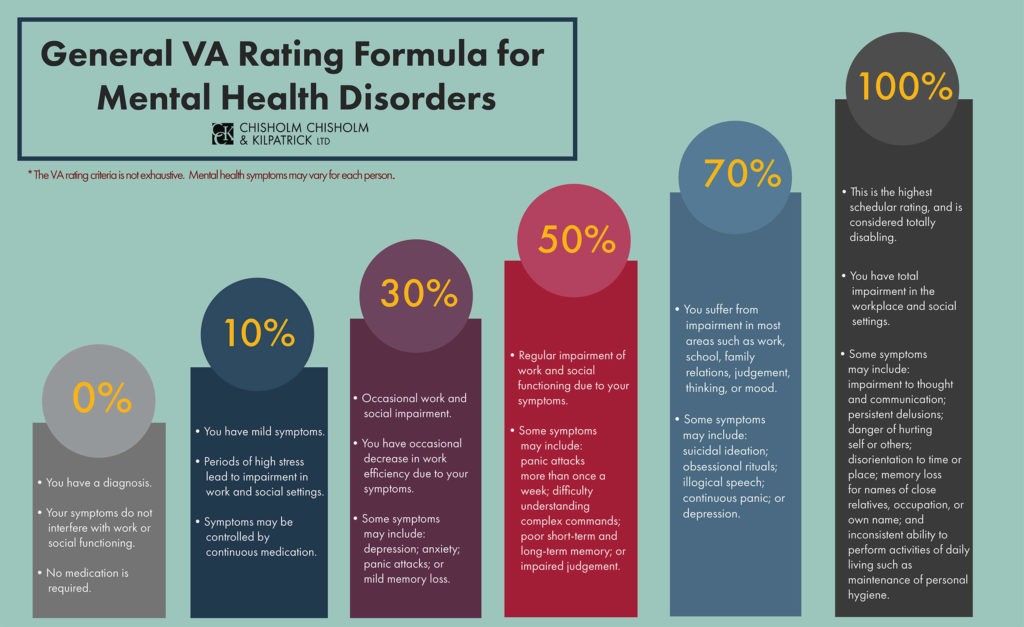
Depression is rated as a mental health condition, as is PTSD, meaning that they are rating with the same formula. Under 38 CFR § 4.130, VA’s General Rating Formula for Mental Health Disorders, veterans can receive a rating of 0, 10, 30, 50, 70, or 100 percent for a mental health condition. Below are the criteria for each rating:
- 100% – total occupational and social impairment, due to such symptoms as: gross impairment in thought processes or communication; persistent delusions or hallucinations; grossly inappropriate behavior; persistent danger of hurting self or others; intermittent inability to perform activities of daily living (including maintenance of personal hygiene); disorientation to time or place; memory loss for names of close relatives, own occupation, or own name
- 70% – occupational and social impairment, with deficiencies in most areas, such as work, school, family relations, judgment, thinking, or mood, due to such symptoms as: suicidal ideation; obsessional rituals which interfere with routine activities; speech intermittently illogical, obscure, or irrelevant; near-continuous panic or depression affecting the ability to function independently, appropriately and effectively; impaired impulse control; spatial disorientation; neglect of personal appearance and hygiene; difficulty in adapting to stressful circumstances (including work or a work-like setting); inability to establish and maintain effective relationships
- 50% – occupational and social impairment with reduced reliability and productivity due to such symptoms as: flattened affect, circumstantial circumlocutory, or stereotyped speech; panic attacks more than once a week; difficulty in understanding complex commands; impairment of short- and long-term memory; impaired judgment; impaired abstract thinking; disturbances of motivation and mood; difficulty in establishing and maintaining effective work and social relationships
- 30% – occupational and social impairment with occasional decrease in work efficiency and intermittent periods of inability to perform occupational tasks (although generally functioning satisfactorily, with routine behavior, self-care, and conversation normal), due to such symptoms as: depressed mood, anxiety, suspiciousness, panic attacks (weekly or less often), chronic sleep impairment, mild memory loss (such as forgetting names, directions, recent events)
- 10% – occupational and social impairment due to mild or transient symptoms which decrease work efficiency and ability to perform occupational tasks only during periods of significant stress, or symptoms controlled by continuous medication
- 0% – a mental condition has been formally diagnosed, but symptoms are not severe enough either to interfere with occupational and social functioning or to require continuous medication
Importantly, a veteran does not need to meet all the symptoms listed in a specific rating in order to receive that rating.

Anxiety Secondary to PTSD
Anxiety—Anxiety is a mental health condition that is defined as intense, excessive, and persistent worry and fear about everyday situations.
There are several types of anxiety disorders, such as generalized anxiety disorder, panic disorder, and various phobia-related disorders. People with any form of these disorders may feel restless or jumpy, have difficulty concentrating, tremble or twitch, feel nauseous or dizzy, experience a rapid heartbeat, have shortness of breath, have difficulty sleeping, or experience excessive worrying.
There are several different diagnostic codes used for different forms of anxiety, specifically:
- DC 9400: Generalized anxiety disorder
- DC 9403: All phobias, including social anxiety disorder
- DC 9404: Obsessive-compulsive disorder
- DC 9410: Other specified anxiety disorder
- DC 9411: Post-traumatic stress disorder
- DC 9412: Panic disorder and/or agoraphobia
Although there are different diagnostic codes used for different anxiety disorders, the rating criteria is the same, since all the codes are rated under the General Rating Formula for Mental Disorders included in 38 CFR § 4.130.
Veterans can receive ratings at 0, 10, 30, 50, 70, or 100 percent and the criteria is the same as the above criteria listed for depression ratings. Be aware, however, that a veteran cannot receive separate ratings for all three conditions (anxiety, depression, and PTSD) since they are all rated under the same rating criteria, as this is called pyramiding.
GERD Secondary to PTSD
GERD—GERD, or Gastroesophageal Reflux Disease, is a digestive disorder characterized by the occurrence of stomach acid flowing back up the esophagus from the stomach, causing discomfort and inflammation.
GERD is caused by frequent episodes of acid reflux. Common symptoms can include heartburn, difficulty swallowing, regurgitation, and chest pain.
Typically, GERD is rated analogously to a hiatal hernia under 38 C.F.R. 4.114 diagnostic code 7346. Veterans can receive a rating for GERD at 10, 30, or 60 percent. The rating criteria for GERD are as follows:
- 10% rating—For this rating, a veteran must present with “two or more symptoms of the 30 percent evaluation of less severity.”
- 30% rating— This rating requires “persistently recurrent epigastric distress with dysphagia, pyrosis, and regurgitation, accompanied by substernal or arm and shoulder pain, productive of considerable impairment of heath.”
- 60% rating—The 60 percent rating requires “symptoms of pain, vomiting, material weight loss and hematemesis or melena with moderate anemia; or other symptom combinations productive of severe impairment of health.”

Hypertension Secondary to PTSD
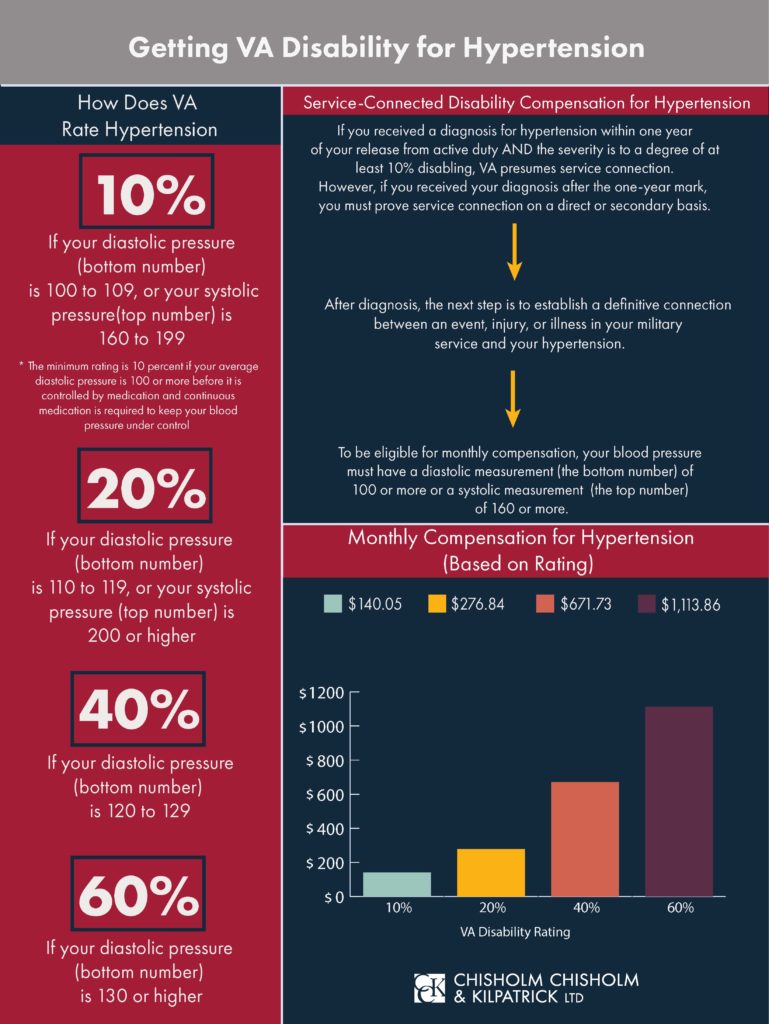
Hypertension—Hypertension means high blood pressure that is consistently above normal. Blood pressure is the pressure of blood pushing against the walls of your arteries. Blood pressure is measured with two numbers:
- Systolic blood pressure – measures the pressure in your arteries when your heart beats
- Diastolic blood pressure – measures the pressure in your arteries when your heart rests between beats
High blood pressure places people at higher risk for other health problems like heart disease, heart attack, and stroke. Research indicates that hypertension may be aggravated by stress and anxiety, which are very common with PTSD symptoms.
Generally, a normal blood pressure level is less than 120 systolic and 80 diastolic. VA acknowledges high blood pressure as 160 or higher for systolic and 90 or higher for diastolic.
Veterans may be rated at 10, 20, 40, or 60 percent for their hypertension under 38 CFR § 4.104 – Schedule of Ratings, Cardiovascular System, Diagnostic Code 7101. The criteria are as follows:
- 60% – diastolic pressure predominantly 130 or more
- 40% –diastolic pressure predominantly 120 or more
- 20% –diastolic pressure predominantly 110 or more, or; systolic pressure predominantly 200 or more
- 10% –diastolic pressure predominantly 100 or more, or; systolic pressure predominantly 160 or more, or; minimum evaluation for an individual with a history of diastolic pressure predominantly 100 or more who requires continuous medication for control
Migraines Secondary to PTSD
Migraines—Migraines are a form of headache that can last for many hours and can bring pain, nausea, vomiting, sensitivity to light and sound, lightheadedness, and blurred vision.
Migraines can also create a throbbing sensation on either side of the head. Sometimes an aura, which is categized by visual disturbances such as flashes of light, may come before a migraine.
There is no singular, definitive cause of migraines, but triggers are thought to include hormonal imbalance, alcohol, stress, sensory stimulation, certain foods, and changes in environment. As stress can trigger migraines, veterans with PTSD often suffer from migraines as well.
Migraines are rated under 38 C.F.R. 4.124a, Diagnostic Code 8100. Veterans can receive ratings for migraines from 0 to 50 percent, with criteria based on severity and frequency of the migraines. Below are the criteria for each rating:
- 50% – with very frequent completely prostrating and prolonged attacks productive of severe economic inadaptability
- 30% – with characteristic prostrating attacks occurring on an average of once a month over the last several months
- 10% – with characteristic prostrating attacks averaging one in two months over the last several months
- 0% – with less frequent attacks
Erectile Dysfunction (ED) Secondary to PTSD
Erectile Dysfunction—Erectile dysfunction, or ED, is defined as difficulty getting or keeping an erection firm enough for sexual intercourse.
Some veterans can experience ED as a result of the emotional stress caused by their PTSD, while others may find ED to be a side effect of PTSD medication.
There is no specific disability rating for erectile dysfunction. Instead, VA rates the condition under 38 C.F.R. § 4.115b. The rating codes used may be:
- Code 7520: If doctors removed half or more than half of your penis, you receive a rating of 30 percent.
- Code 7521: If doctors removed your glans, your rating is 20 percent.
- Code 7522: If your penis cannot become erect because of a physical deformity, you receive a 20-percent rating.
- Code 7523: If your erectile dysfunction is due to atrophied testicles, a condition often resulting in reduced testosterone and thus a lower sex drive, you receive a 20-percent rating if the condition affects both testicles, and a 0 percent rating if it affects only one testicle.
- Code 7524: If you had both testicles removed due to a service-connected event, you receive a 30-percent rating; if you had one testicle removed due to a service-connected event, you receive a 0-percent rating.
Generally, the VA will grant a 0-percent rating for erectile dysfunction unless you are eligible under the diagnostic codes above. However, service connection for erectile dysfunction, even at 0 percent, makes veterans eligible for Special Monthly Compensation (SMC) for loss of use of a creative organ. This is known as SMC (k) and is paid out in your monthly VA compensation check.
TDIU for PTSD and Secondary Conditions
If your PTSD and other related conditions significantly impair your ability to work, you may be eligible for a total disability rating based on individual unemployability (TDIU).
TDIU allows veterans to receive compensation at the 100 percent rate if their service-connected condition(s) prevent them from securing and maintaining substantially gainful employment.
VA outlines TDIU regulations under 38 CFR § 4.16, which encompasses subsections (a) and (b). Each subsection describes the ways in which veterans can meet the eligibility requirements for TDIU. In order to qualify for TDIU under 38 CFR § 4.16(a), or schedular TDIU, a veteran must have:
- One service-connected condition rated at 60 percent or higher; or
- Two or more service-connected conditions, one of which is rated at 40 percent or higher, with a combined rating of 70 percent or higher.
If a veteran has a rating for PTSD, and a rating for a secondary condition to PTSD, the secondary rating can contribute to their overall combined disability rating and help to make the veteran eligible for schedular TDIU.
Veterans who do not meet the schedular requirements under 38 CFR § 4.16(a) may still be considered for extraschedular TDIU under § 4.16(b). Extraschedular TDIU does not have any rating requirement. If veterans do not meet the criteria for schedular TDIU, VA will determine if their case should be referred to the Director of Compensation Service for extraschedular consideration.
Was Your VA Claim Denied, or Were You Under-Rated?
If you need help with your claim for secondary service connection related to PTSD, CCK may be able to help. Our experienced team has helped veterans establish secondary service connection for conditions related to PTSD and receive the benefits they deserve. Call our office today at 800-544-9144 for a free case evaluation.
About the Author
Share this Post