VA Disability Ratings for Restless Leg Syndrome (RLS)

CCK Law: Our Vital Role in Veterans Law
Restless leg syndrome (RLS) is a frustrating neurological condition that causes discomfort in a veteran’s legs. This disorder commonly interferes with sleep and can lead to exhaustion or fatigue, negatively affecting a veteran’s day-to-day life.
Veterans with restless leg syndrome may qualify for compensation and disability benefits from the Department of Veterans Affairs (VA) if their condition was caused by service OR caused by another service-connected condition. This article will explore the link between military service and RLS and what steps you can take to ensure you receive the compensation you deserve.
In this article, you will discover:
- What restless leg syndrome is and how it is caused
- How to establish service connection for your restless leg syndrome
- VA disability compensation and benefits for restless leg syndrome
- And more
What Is Restless Leg Syndrome?
Restless leg syndrome, or Willis-Ekbom Disease, is a condition that can cause painful and uncomfortable sensations in the legs. These sensations occur most commonly in the late afternoon or evening and can become particularly excruciating at night. Other symptoms may include:
- The irresistible urge to move your legs
- Itching, shocking, aching or throbbing in the legs
- Leg twitching
- Fatigue
- Muscle atrophy from sleep disruption (sarcopenia)
The nature of RLS can make it difficult to sleep at night, whether it be falling asleep or returning to sleep once having been awoken. Moving one’s legs may provide relief to the discomfort, but the unpleasant sensations may return once the movement has stopped. Walking may also provide temporary relief.
Notably, the lack of sleep caused by RLS can lead to serious consequences. Sleep deprivation can affect a person’s mood, personal relationships, and overall ability to function. Often, people who experience RLS also find that they have difficulty concentrating, impaired memory, and decreased work productivity, as well as anxiety and depression. In moderate or severe cases, the absence of restful sleep can even lead to substantial muscle atrophy, or sarcopenia.
What Causes Restless Leg Syndrome?
Ultimately, the true cause of RLS is still unknown to doctors. Some experts classify it as a sleep disorder and a movement disorder, as the symptoms are brought on by sleep and lack of movement. Others characterize it as a neurological sensory disorder because the symptoms are produced by the brain.
Despite this uncertainty, there are risk factors and comorbid conditions that can increase your chance of receiving a diagnosis of restless leg syndrome:
- Family history of RLS
- Dysfunction of the basal ganglia
- Parkinson’s disease
- Sleep apnea or deprivation
- End-stage renal disease
- Iron deficiency
- Neuropathy
- Use of certain medications (including antinausea medications, antipsychotic medications, antidepressants, and allergy medication)
- Use of alcohol, nicotine, and caffeine
- Pregnancy
- Exhaustion and daytime sleepiness
- Post-traumatic stress disorder (PTSD)
RLS affects men and women, although it affects women more commonly than men. The symptoms can also worsen and become more frequent with age.
Restless Leg Syndrome and Periodic Limb Movements of Sleep (PLMS)
Another significant condition that often co-exists with RLS is something called periodic limb movements of sleep (PLMS) or periodic limb movement disorder (PLMD). This disorder causes a patient’s arms and legs to involuntarily twitch during the night, typically every 20-40 seconds.
As many as 80-90 percent of RLS patients may also have some degree of PLMS. Though the exact link between the conditions is unclear, they share risk factors like iron deficiency, sleep apnea, and nerve damage.
Treating RLS
Though restless leg syndrome may subside with time, there are some treatments that may be used to reduce the discomfort.
- Reduced Exercise—Reducing the level of exercise may ease the pain of RLS. Additionally, warm baths, leg massages, heating, and icing the legs may provide additional relief.
- Lifestyle changes—Some lifestyle changes may help reduce symptoms of RLS. Specifically, ceasing to use alcohol and tobacco, as well as maintaining a consistent sleep schedule, could help reduce the recurrence of RLS and alleviate symptoms.
- Medications—Specific medications may be used to treat RLS, such as anti-seizure drugs and dopaminergic agents.
- Iron supplements—RLS may occur in individuals who have low iron levels in their blood. Iron supplements may be used to increase an individual’s iron levels, which in turn may help treat RLS.
Establishing VA Service Connection for Restless Leg Syndrome
RLS can be the result of several diseases or injuries that are common to veterans. Some of these conditions include:
- Traumatic brain injury (TBI) or nerve damage: Brain and spinal cord injuries are not uncommon among veterans, due to the often physically demanding nature of their military service. Unfortunately, these injuries can lead to significant nerve damage—or neuropathy—which is a large risk factor for developing RLS.
- Post-traumatic stress disorder (PTSD): Many veterans suffer from PTSD and other panic or anxiety disorders. With the stress, chemical changes, and sleep deprivation these conditions provoke, some patients go on to develop restless leg syndrome as a result.
- Sleep apnea: Among veterans, sleep apnea often develops due to factors like PTSD or exposure to toxic chemicals. As sleep becomes more difficult and less restful, these veterans gain an increased chance of being diagnosed with RLS.
To receive VA disability benefits for restless leg syndrome, a veteran must first prove there is a link between their RLS and their military service. This is called a service connection, and veterans can establish it in multiple ways.
Direct Service Connection for Restless Leg Syndrome
A direct service connection is when a veteran can prove that their RLS directly resulted from or was aggravated by something that happened during their military service.
To establish this direct link and potentially claim VA disability benefits for restless leg syndrome, a veteran will need three things:
- A current diagnosis of restless leg syndrome;
- An in-service injury, event, or illness that caused or aggravated the RLS; and
- A medical nexus that links the veteran’s RLS to their service.
To file a claim, veterans may use VA Form 21-526EZ, which has sections regarding the veteran’s service, condition, and identifying information. Veterans may also wish to include information regarding the severity of their condition. Restless leg syndrome can range drastically in severity, and some veterans may not recognize they have it.
Secondary Service Connection and Restless Leg Syndrome
Secondary service connection can be granted when a condition arises or is aggravated by an already service-connected condition. Veterans may be awarded secondary service connection disability benefits for RLS in instances where an already service-connected condition caused or worsened the veteran’s restless leg syndrome.
For example, if a veteran has been service-connected for sleep apnea and their sleep apnea causes or aggravates RLS, the veteran can file a claim for secondary service connection. Conversely, if the veteran has been service-connected for RLS and it causes or aggravates their sleep apnea, they may also file for secondary service connection.
The nature of RLS can make it difficult to determine whether the condition is caused by another condition or whether it causes another condition. Additionally, sometimes it can take years for restless leg syndrome to manifest or for a veteran to realize that they suffer from RLS.
To prove secondary service connection, the veteran will need an opinion from a doctor or medical professional that links the service-connected condition to the claimed secondary condition. The opinion should state how the two conditions are linked. Additionally, the veteran will need a current medical diagnosis for the claimed secondary condition.
VA Presumptions for Restless Leg Syndrome
Under certain circumstances, VA may automatically presume that a veteran’s condition is connected to their military service. Typically, this makes the claims process much simpler and easier to handle.
VA recognizes only one set of circumstances that establishes this presumptive connection for restless leg syndrome: the veteran must manifest symptoms of RLS during or within one year of their departure from military service, and these symptoms must be rated at a degree of 10 percent or more.
If these conditions are met, VA will more than likely determine a veteran’s RLS is indeed a result of their service.
Compensation and Pension (C&P) Exams for Restless Leg Syndrome
VA may request a Compensation and Pension (C&P) exam once a claim has been filed for restless leg syndrome. The C&P exam for restless leg syndrome will be performed by a VA physician or a VA-contracted physician. Prior to the exam, the examiner should review the veteran’s c-file, which contains the veteran’s medical and service records.
It is important to attend the exam, as failing to attend or to follow through with scheduling the exam could result in a denial of the veteran’s claim.
During the exam, the examiner may ask the veteran questions about their restless leg syndrome or about their military service. They may also physically examine the veteran.
The veteran may also use a DBQ, or Disability Benefits Questionnaire, to bolster their claim. A Disability Benefits Questionnaire is a form created by VA so that the veteran may address important aspects of their condition, such as symptoms, severity, possible causes, and relation to other disabilities. For restless leg syndrome, veterans may use the Disability Benefits Questionnaire for knee and lower leg conditions.
How VA Rates Restless Leg Syndrome for Disability Benefits
VA issues ratings for restless leg syndrome for each individual leg affected. The ratings start at 10 percent and increase based on severity.
For veterans trying to become rated for RLS, VA will often consider additional evidence before issuing its decision. This could include the number of times a veteran has sought treatment and how effective treatment has been.
VA rates restless leg syndrome by “analogy” under Diagnostic Code 8620, which relates to neuritis of the sciatic nerve, or occasionally Diagnostic Code 8103 for convulsive tics. The ratings range from mild to severe.
Neuritis of the Sciatic Nerve
- Mild – 10%
- Moderate – 20%
- Moderately Severe – 40%
- Severe – 60%
Convulsive Tics
The rating is determined by the frequency and severity of the spasms, as well as the muscle groups involved.
- Mild – 0% for mild
- Moderate – 10%
- Severe – 30%
TDIU and Restless Leg Syndrome
Another benefit that may be available to veterans who experience restless leg syndrome is total disability based on individual unemployability, or TDIU. This disability benefit is available to veterans who may not regularly meet the criteria needed to reach the 100 percent rating.
Veterans who are service-connected for RLS may be eligible for this benefit. There are generally two pathways to become eligible for TDIU:
- 38 CFR § 4.16a(“Schedular”) – For this form of TDIU, the veteran must have:
- One condition rated at a minimum of 60 percent OR
- Two conditions combined to reach 70 percent, where one condition is rated at a minimum of 40 percent.
- 38 CFR § 4.16b(“Extraschedular”) – This form of TDIU is for veterans who may not be able to achieve the ratings necessary for schedular TDIU but are still unable to obtain substantially gainful employment on account of their conditions. In this instance, the veteran must prove that their condition uniquely hinders their ability to obtain substantially gainful employment and therefore should not be rated on the standard disability rating criteria.
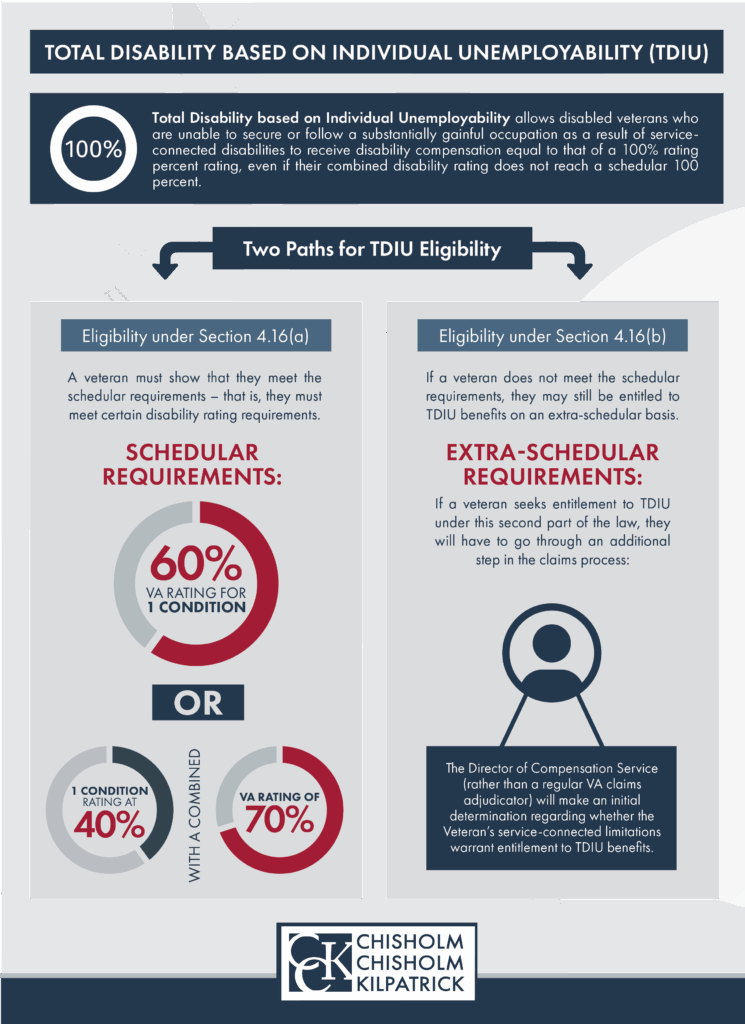
The rating given for a veteran’s restless leg syndrome may be combined with a rating for another condition to help the veteran meet the criteria for schedular TDIU.
Was Your VA Disability Claim Denied?
Often, claims for RLS can be difficult to win due to the nature of the condition. If your VA disability claim for restless leg syndrome has been denied, the VA disability lawyers at Chisholm, Chisholm & Kilpatrick may be able to help. Contact us today at 800-544-9144.
About the Author
Share this Post
