VA Disability Ratings for Pancreatic Cancer

Veterans who developed pancreatic cancer from their military service may be eligible to receive VA disability benefits for their cancer. Pancreatic cancer may develop in veterans who have been exposed to certain toxins during their service, particularly those who were exposed to radiation or military burn pits.
What is Pancreatic Cancer?
Pancreatic cancer is caused by abnormal cells in the pancreas, which can grow and divide to form a tumor. The pancreas itself is made up of cells that, normally, divide to form new cells as the body needs them. This usually happens when old cells die, as new ones take their place.
The pancreas itself is a gland in the abdomen, which rests between the stomach and the spine. The pancreas produces enzymes that aid digestion and hormones that control blood sugar levels.
Tumors in the pancreas may form when old cells do not die as intended. These extra cells can then form a mass or tumor. Tumors can be benign, meaning that they are abnormal but do not invade any other parts of the body. Other tumors may be malignant, meaning they are cancerous. In malignant tumors, the cells can spread to other parts of the body, including tissues and organs. Often, pancreatic cancer spreads to the liver, lungs, bones, or lymph nodes.
Types of Pancreatic Cancer
- Adenocarcinoma—This is the most common form of pancreatic cancer. About 9 out of 10 people who have been diagnosed with pancreatic cancer have this form. Adenocarcinoma is an exocrine tumor, meaning the cancer starts in the cells lining the pancreatic duct. The cells there are responsible for making enzymes for digestion.
- Acinar Cell Carcinoma—This form of pancreatic cancer is very rare. Specifically, these tumors may cause the pancreas to create too much lipase. Lipase is an enzyme that digests fats and can be measured in the blood.
- Intrapapillary papillary-mucinous neoplasm (IPMN) —This tumor may grow in the pancreatic duct, or in the side branches of the duct. The tumor can be benign, but also has a chance of becoming cancerous. The risk of the tumor being malignant is higher if the tumor is in the pancreatic duct.
- Mucinous cystic neoplasm with an invasive adenocarcinoma —This type of tumor is also rare. In this form of pancreatic cancer, a cyst may form in the tail for the pancreas. Most commonly, this form affects women. If the cancer is not invasive, it is most likely benign.
- Neuroendocrine Tumors—Unlike the above forms of pancreatic cancer, which are exocrine tumors, neuroendocrine tumors are another type. Neuroendocrine tumors make up about 7 percent of pancreatic tumors. Neuroendocrine tumors are also referred to as islet cell tumors, or pancreatic NETs or PNETs. Usually, they grow slower than exocrine tumors. These tumors come from the abnormal growth of endocrine cells, which create the hormones that control blood sugar levels. These tumors are either functional or nonfunctional. If they are functional then they will produce hormones, whereas nonfunctional tumors do not produce hormones. Forms of pancreatic neuroendocrine tumors include: gastrinoma, glucagonoma, insulinoma, somatostatinoma, VIPoma, and nonfunctional islet cell tumor.
Symptoms
- Stomach or back pain
- Weight loss
- Loss of appetite
- Nausea
- Changes in stool
- Pancreatitis, or swelling in the pancreas
- Jaundice, in the skin or eyes
- Itching in the skin
- Recent-onset diabetes
Diagnosis and Treatment
The only way to diagnose pancreatic cancer is through imaging such as a CT scan, MRI, or endoscopic ultrasound. A doctor may also sample the tissue of the tumor to analyze it.
The treatments available for pancreatic cancer depend on what stage the cancer is in and the overall health of the infected person. Standard treatments to treat pancreatic cancer include surgery, chemotherapy, and radiation. Treatment can become complicated, however, as patients who are diagnosed with pancreatic cancer at later stages are not eligible for surgery, which is one of the more effective treatments. This is one of the reasons why early detection of this condition can be so crucial.
Additionally, the stroma, or the tissue surrounding pancreatic tumors, is often very dense. This can make it difficult for treatment to reach the tumor.
Causes
Pancreatic cancer can be hereditary, meaning that it can be inherited from one’s parents, or it can arise over time. Additionally, exposure to something harmful can cause pancreatic cancer. For veterans who develop pancreatic cancer, this could be caused by exposure to toxins from military burn pits. Pancreatic cancer may also develop randomly.
Some risk factors can also include a person’s race, age, and sex. If a person has long-standing diabetes, or a history of smoking, they may face a higher risk of developing pancreatitis. Obesity and a diet high in red and processed meat can also pose a risk.
VA Service Connection for Pancreatic Cancer
When filing a claim for service connection for pancreatic cancer, the veteran will need to demonstrate a connection between their military service and their pancreatic cancer. The veteran will also need to submit a diagnosis of their pancreatic cancer. In general, the veteran will need to submit the following to VA:
- A diagnosis of pancreatic cancer;
- An in-service event, illness, or injury; and
- A nexus linking the veteran’s in-service occurrence with their pancreatic cancer.
In instances of presumptive service connection, a veteran may not need to submit a nexus linking their in-service occurrence with their pancreatic cancer.
To support the veteran’s claim for service connection, the veteran may submit lay evidence. Lay evidence, or lay statements, can be written by the veteran or anyone who knows the veteran and can speak to their condition. Importantly, lay evidence may also be submitted by fellow service members. For veterans with pancreatic cancer, fellow service members may be able to speak to the veteran’s exposure during their service.
Compensation and Pension (C&P) Exams for Pancreatic Cancer
When a veteran files a claim for pancreatic cancer, VA may request a Compensation and Pension exam, or C&P exam. To do this, VA may call the veteran or send a letter. It is very important to make sure VA has the most up-to-date contact information so that the veteran does not miss any C&P exam requests. It is also crucial to attend the exam, as failure to do so can result in VA denying the veteran’s claim.
The exam will usually be performed by a VA physician or a VA contracted physician. Before the exam, the examiner will review the veteran’s c-file, which contains any documentation that has previously been submitted to VA, as well as the veteran’s medical and service records. The examiner may physically examine the veteran or ask questions regarding their condition or symptoms.
The veteran may also use a DBQ, or Disability Benefits Questionnaire, to bolster their claim. A Disability Benefits Questionnaire is a form created by VA so that the veteran may address important aspects of their condition, such as symptoms, severity, possible causes, and relation to other disabilities. The veteran may also have their private doctor fill out a DBQ for them. In claims for pancreatic cancer, DBQs can be helpful because a private doctor who treats the veteran’s cancer can provide a more in-depth analysis of the veteran’s condition.
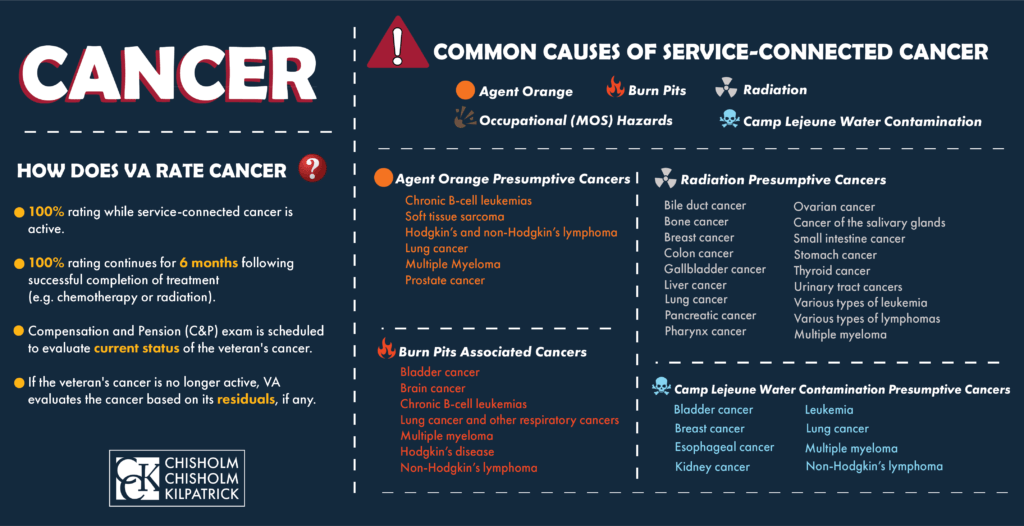
VA Ratings for Pancreatic Cancer
If a veteran is service-connected for an active cancer, VA should automatically assign a 100 percent disability rating. This rating will continue as long as the veteran’s cancer is active. After six months following the veteran’s successful treatment program, which can include chemotherapy, radiation, or surgery, VA will schedule the veteran for another C&P exam to re-evaluate their condition. If the veteran’s cancer is in remission, then VA will evaluate the cancer based on its residuals.
Toxic Exposure and Pancreatic Cancer
Pancreatic cancer has been linked to veterans who were exposed to certain chemicals or toxins during their service. Some of these forms of exposure have presumptive service connection, meaning that the veteran does not have to prove a connection between their pancreatic cancer and their service, while others do not.
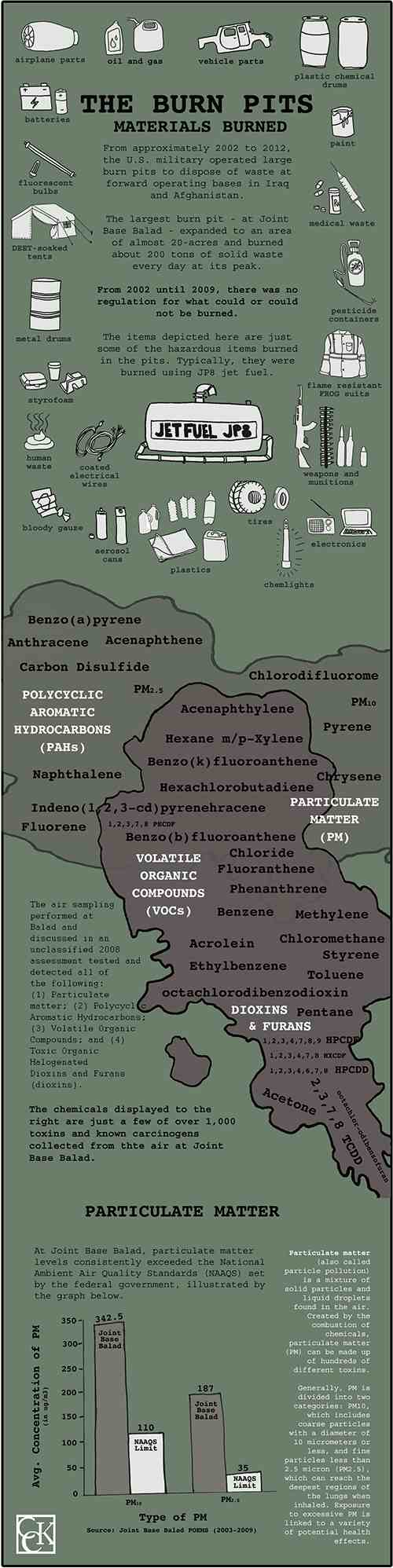
Burn Pit Exposure and Cancer
Military burn pits are large areas of land in which the military and its contractors incinerated all waste generated by military bases. The United States military used burn pits as part of its waste disposal protocol in places such as Iraq and Afghanistan in the post-9/11 era. The practice was effective in reducing large quantities of waste, but the pits emitted plumes of toxic smoke. Materials such as human and medical waste, plastic, rubber, petroleum, and ammunition were disposed of in burn pits.
As of the Honoring Our Promise to Address Comprehensive Toxics Act (PACT Act) of 2021, VA currently provides presumptive service connection for pancreatic cancer for “covered veterans” exposed to burn pits and other toxins during military service. A covered veteran is defined as the following:
- A veteran who, on or after August 2, 1990, performed active military, naval, air, or space service while assigned to a duty station in, including air space above:
- Bahrain
- Iraq
- Kuwait
- Oman
- Qatar
- Saudi Arabia
- Somalia
- United Arab Emirates
- A veteran who, on or after September 11, 2001, performed active military, naval, air, or space service, while assigned to a duty station, including the airspace above:
- Afghanistan
- Djibouti
- Egypt
- Jordan
- Lebanon
- Syria
Veterans who served in one of the above locations during a qualifying time period and who developed sarcoidosis can qualify for presumptive service connection without needing to provide a nexus. This makes is significantly easier to secure VA disability compensation for their condition.
When President Biden officially signed the PACT Act into law, he and VA Secretary McDonough announced that the rollout period for certain presumptive conditions for covered veterans would be waived. Initially, these presumptions were effective upon the date of enactment of the PACT Act only for certain conditions, while presumptions for other conditions would become effective on a rolling basis over the next few years. Now, with this new rollout plan, the presumption for all conditions are effective from the date the PACT Act was signed (August 10, 2022) and VA will begin adjudicating these claims as soon as January 2023. Veterans should know, however, that newly eligibly claimants will not get retroactive benefits back to the date of their original claim unless they are filing a claim for DIC benefits.
Radiation Exposure
Ionizing radiation includes gamma rays, x-rays, and higher ultraviolet parts of the electromagnetic spectrum. “Atomic Veterans” refers to veterans who participated in “radiation-risk activity” and may have been exposed to this radiation. According to VA, veterans who served in the following locations may have been exposed to ionizing radiation:
- Occupation of Hiroshima and Nagasaki, Japan from August 6, 1945 and July 1, 1946
- Prisoners of War (POWs) in Japan during World War II
- Participants in atmospheric nuclear weapons tests, primarily conducted in Nevada and the Pacific Ocean from 1945 to 1962
- Underground nuclear weapons testing in Amchitka Island, Alaska prior to January 1, 1974
- Any of the following gaseous diffusion plants for at least 250 days prior to February 1, 1991:
- Paducah, Kentucky
- Portsmouth, Ohio
- K25 in Oak Ridge, Tennessee
- “Worked as an x-ray technician, in a reactor plant, or in nuclear medicine or radiography”
- “Did tasks like those of a Department of Energy (DoE) employee that makes them a member of the Special Exposure Cohort”
Additional circumstances in which veterans may have been exposed include:
- The Fukushima nuclear accident in Japan from March 12 to May 11, 2011
- The U.S. Air Force plutonium clean-up mission in Palomares, Spain
- Exposure to depleted uranium
- Exposure to radiation from Long Range Navigation stations (LORAN) from 1942 to 2010
- McMurdo Station, Antarctica nuclear power plant from 1964 to 1973
Furthermore, the PACT Act added the following presumptive locations for veterans exposed to radiation:
- Enewetak Atoll from January 1, 1977 to December 31, 1980
- The response to the Palomares, Spain B-52 plane crashfrom January 17, 1966 to March 31, 1967
- The response to the B-52 plane crash at Thule Air Force Base in Greenlandfrom January 21, 1968 to September 25, 1968.
Pancreatic cancer has been associated with exposure to ionizing radiation. As such, VA recognizes presumptive service connection for veterans who developed pancreatic cancer as a result of their exposure to radiation. This means that the veteran is not required to provide a medical nexus linking their condition to the exposure.
Agent Orange Exposure and Pancreatic Cancer
While VA does not presume pancreatic cancer as connected to exposure to Agent Orange, veterans can still prove their claim on a case-by-case basis with a supporting medical nexus, potentially lay testimony, and more.
Getting Help with Service Connection for Pancreatic Cancer
Even though pancreatic cancer does have presumptive service connection in some instances, the process can be confusing and difficult for veterans to navigate on their own. An accredited representative or lawyer may be able to assist veterans with their appeals for pancreatic cancer. The VA disability lawyers at Chisholm, Chisholm & Kilpatrick may be able to help with your appeal. For a free case evaluation, call our office at 800-544-9144.
About the Author
Share this Post