Testicular Cancer VA Disability Claims and Ratings

CCK Law: Our Vital Role in Veterans Law
Testicular cancer is a condition that affects many veterans as a result of their military service. VA offers service-connected compensation to these veterans based on the active cancer or the presence and severity of the cancer residuals.
What is Testicular Cancer?
Cancer occurs when cells in the body grow out of control. Testicular cancer occurs when the cells grow out of control in the testicles specifically. The testicles, or testes, are part of the male reproductive system. The two main functions of the testicles are to produce male hormones, such as testosterone, and to create sperm.
Forms of Testicular Cancer
There are multiple forms of testicular cancer, as the testicles are made up of many different kinds of cells.
- Germ Cell Tumors—Most testicle cancers begin as germ cells. The germ cells are the cells responsible for making sperm. There are two sub-types of germ cell tumors: seminomas and non-seminomas. Testicular cancer can involve one or more of both kinds of these germ cell tumors.
- Seminomas—Seminomas grow slower than non-seminomas. These tumors may increase the production of a protein called human chorionic gonadotrophin. There are also sub-types of seminomas.
- Non-seminomas—Non-seminomas spread more quickly than seminomas. There are four sub-types of non-seminomas: embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma.
- Carcinoma in situ of the testicle—In some cases, testicular germ cell cancer may begin as carcinoma in situ. The cells will look abnormal under a microscope, but they typically do not spread into other areas, such as where the sperm cells are formed. This form of testicular germ cell cancer does not always progress into invasive cancer.
- Stromal tumors—Stroma are hormone-producing tissue. Tumors can begin in the stroma, but they are uncommon. There are also two forms of stromal tumors.
- Leydig cell tumors—Leydig cells make male sex hormones, such as testosterone. Leydig cell tumors may also make estrogen, a female sex hormone. Frequently, Leydig cell tumors are benign, meaning they are not cancerous. They may spread to other parts of the body beyond the testicles and do not respond well to treatment.
- Sertoli cell tumors—Sertoli cells aid the sperm-making germ cells. Similar to Leydig cell tumors, these tumors are usually benign but, when cancerous, they do not respond well to treatment.
- Secondary testicular cancer—Some cancers can begin in other areas of the body and eventually spread to the testicles. These cancers are named based on the organ of the body in which they start. For example, prostate cancer may begin in the prostate and then spread to the testicles. Lymphoma is the most common secondary testicular cancer.
Symptoms of Testicular Cancer
- Swelling, or the feeling of a lump, in the testicle
- Breast growth, or soreness
- Low back pain
- Shortness of breath
- Chest pain
- Coughing
- Stomach pain
- Headaches
- Confusion
Diagnosis and Treatment
Certain factors could make a person more susceptible to developing testicular cancer. Some risks include:
- Family history of testicular cancer
- HIV infection
- Having an undescended testicle
- Previous history of testicular cancer
- Body size
Testicular cancer is usually found once a person begins displaying symptoms. Tests to detect and diagnose testicular cancer can include:
- Ultrasound
- Blood tests
- Biopsy
- X-rays
- CT scan
- MRI scan
- PET scan
- Bone scan
Treatments may vary depending on the severity of the cancer, as well as the age and overall health of the individual. These treatment methods could include:
- Surgery
- Radiation therapy
- Chemotherapy
- Stem Cell Transplant
How Does VA Rate Testicular Cancer for Disability Benefits?
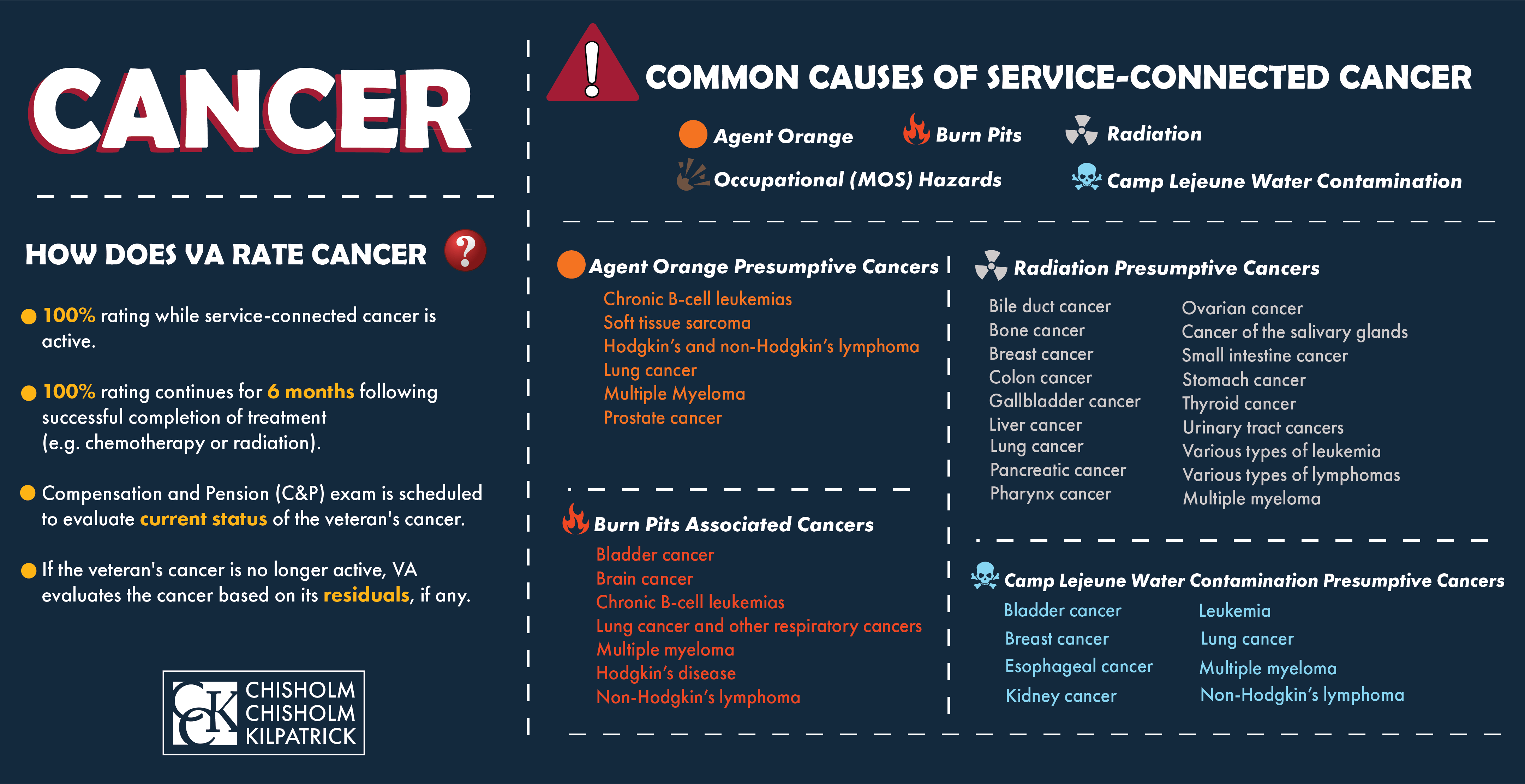
Upon establishing service connection, VA rates testicular cancer depending on if it is active. If the cancer is active, VA should automatically assign a 100 percent disability rating. If the cancer goes into remission, VA will evaluate each residual of the cancer and rate them based on the severity.
These are some common residuals of testicular cancer and their ratings.
- Frequent urination: The rating criteria for urinary frequency ranges from 10 to 40 percent disabling depending on the amount of time between voiding. The 10 percent rating requires “daytime voiding interval between two and three hours, or; awakening to void two times per night.” To qualify for the 40 percent rating, there must be “daytime voiding interval less than one hour, or; awakening to void five or more times per night.”
- Urinary Incontinence: Urinary incontinence is rated under Voiding Dysfunction and includes ratings from 20 to 60 percent disabling. The ratings are dependent on how often a veteran needs their absorbent materials changed due to their incontinence. Absorbent materials include adult diapers or pads, and to be eligible for the 60 percent rating, absorbent materials must be changed four or more times per day.
- Erectile Dysfunction: Erectile dysfunction is a common residual of prostate cancer. VA will only grant 0 percent for erectile dysfunction unless there is deformity with loss of erectile power. However, a grant of service connection for erectile dysfunction deems a veteran eligible for Special Monthly Compensation (SMC) for the loss of use of a creative organ. As of 2021, SMC (k) amounts to $111.74 a month. These are just a few common residuals and some veterans may experience additional residuals. Presence and severity vary from person to person.
Exposure and Testicular Cancer
While many veterans who were exposed to toxins during their service have gone on to develop testicular cancer as a result of their service, VA does not acknowledge presumptive service connection for exposure, as it does with some other forms of cancer.
Agent Orange Exposure
Agent Orange is one of several herbicides, or “rainbow herbicides,” that were used during the Vietnam War era. Specifically, Agent Orange was a mixture of two different kinds of highly toxic chemicals: 2, 4-D and 2, 4, 5-T. The highly toxic dioxin contaminant known as 2, 3, 7, 8-TCDD is a byproduct that is produced by Agent Orange. Many veterans came into contact with Agent Orange, including those who served in areas other than Vietnam.
While VA does acknowledge presumptive service connection for some forms of cancer associated with Agent Orange exposure, such as prostate cancer and bladder cancer, testicular cancer is not recognized. The Institute of Medicine (IOM) has studied the link between Agent Orange and several cancers and has found that there is insufficient evidence of an association between Agent Orange and testicular cancer at this point in time.
Military Burn Pit Exposure
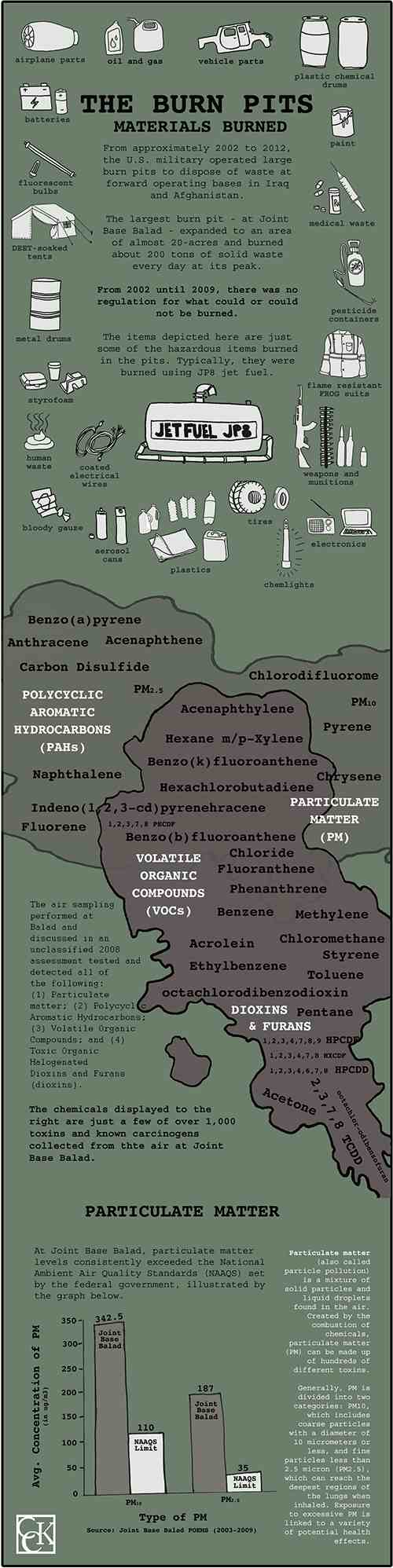
Military burn pits are large areas of land in which the military and its contractors incinerated all waste generated by military bases, including plastics, medical waste, rubber, human waste, and more.
The U.S. Military used burn pits as part of their waste disposal protocol in places such as Iraq and Afghanistan in the post-9/11 era during Operations Iraqi and Enduring Freedom. While the practice was effective in reducing large quantities of waste, burn pits emitted plumes of toxic smoke. This was especially problematic in places such as the Middle East, as the desert wind carried the smoke for miles.
Many U.S. Military veterans have suffered health consequences from burn pit exposure. Most of the negative effects involve temporary ailments of the respiratory system, though limited evidence suggests a link between burn pit exposure and the long-term deterioration of lung health.
These burn pits were used extensively throughout the Middle East and have affected veterans who served in Operation Iraqi Freedom, Operation Enduring Freedom, and Operation New Dawn.
Research continues to be done to link burn pit exposure to a variety of different conditions, such as cancers and respiratory conditions. While further research will need to be conducted, it has indicated that one of the known chemical compounds which was found in Agent Orange, called TCDD, was also released by burn pits. However, unlike some conditions caused by Agent Orange exposure, VA does not acknowledge presumptive service connection for any condition linked to burn pit exposure.
VA does not have a consistent approach to deciding these claims, so lay evidence from veterans is key to winning burn pit claims. Often, VA does not have a way of proving veterans were near burn pits, so statements from the veteran themselves or buddy statements can help verify exposure.
New Proposed Burn Pit Legislation in 2021
As of 2021, there are several major bills currently pending in Congress, that deal with the toxic exposure caused by burn pits. These bills include:
- Conceding Our Veterans’ Exposure Now and Necessitating Training Act (COVENANT)
- Presumptive Benefits for War Fighters Exposed to Burn Pits and Other Toxins Act of 2021
- Veterans Burn Pit Exposure Recognition Act
- Toxic Exposure in the American Military Act (TEAM)
Any of these bills, if passed, would offer much-needed relief to veterans suffering the toxic effects of burn pit exposure. Specifically, the COVENANT Act would make any form of reproductive cancer presumptive. Essentially, this means that the burden of proof would no longer be on the veteran to demonstrate the link between military burn pit exposure and testicular cancer.
Denied VA Disability Benefits for Testicular Cancer?
VA disability claims for testicular cancer may be denied by VA because there is no presumption of exposure or presumptive service connection. However, if your claim for testicular cancer was denied, it does not mean it is the end of the road. Our experienced VA disability attorneys may be able to help you secure VA disability benefits for your testicular cancer. Contact our office today for a free consultation.
About the Author
Share this Post