VA Disability Ratings for Hypertension and Sleep Apnea
CCK Law: Our Vital Role in Veterans Law
To understand VA ratings for hypertension and sleep apnea, it is important to understand the conditions and how they work together.
What is Hypertension?
Hypertension means high blood pressure. According to the Centers for Disease Control and Prevention (CDC), blood pressure is the pressure of blood pushing against the walls of your arteries (i.e., blood vessels that carry blood from the heart to other parts of the body). Blood pressure is measured using two numbers:
- Systolic blood pressure – measures the pressure in your arteries when your heart beats
- Diastolic blood pressure – measures the pressure in your arteries when your heart rests between beats
Generally speaking, a normal blood pressure level is less than 120 systolic and 80 diastolic.
High blood pressure, also referred to as hypertension, is blood pressure that is higher than normal. Blood pressure levels change naturally throughout the day based on your activities; however, having blood pressure that measures consistently above normal may result in a diagnosis of hypertension. This condition is concerning because it places people at higher risk for other health problems, including heart disease, heart attack, and stroke.
Hypertension is typically diagnosed by healthcare providers after reviewing your systolic and diastolic blood pressure levels and comparing them to levels found in certain guidelines. Currently, the Heart Association Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (2017) adheres to the following measurements as they pertain to diagnosing hypertension:
- At-Risk (prehypertension) – systolic: 120-129; diastolic: less than 80
- High Blood Pressure (hypertension) – systolic: 130 or higher; diastolic: 80 or higher
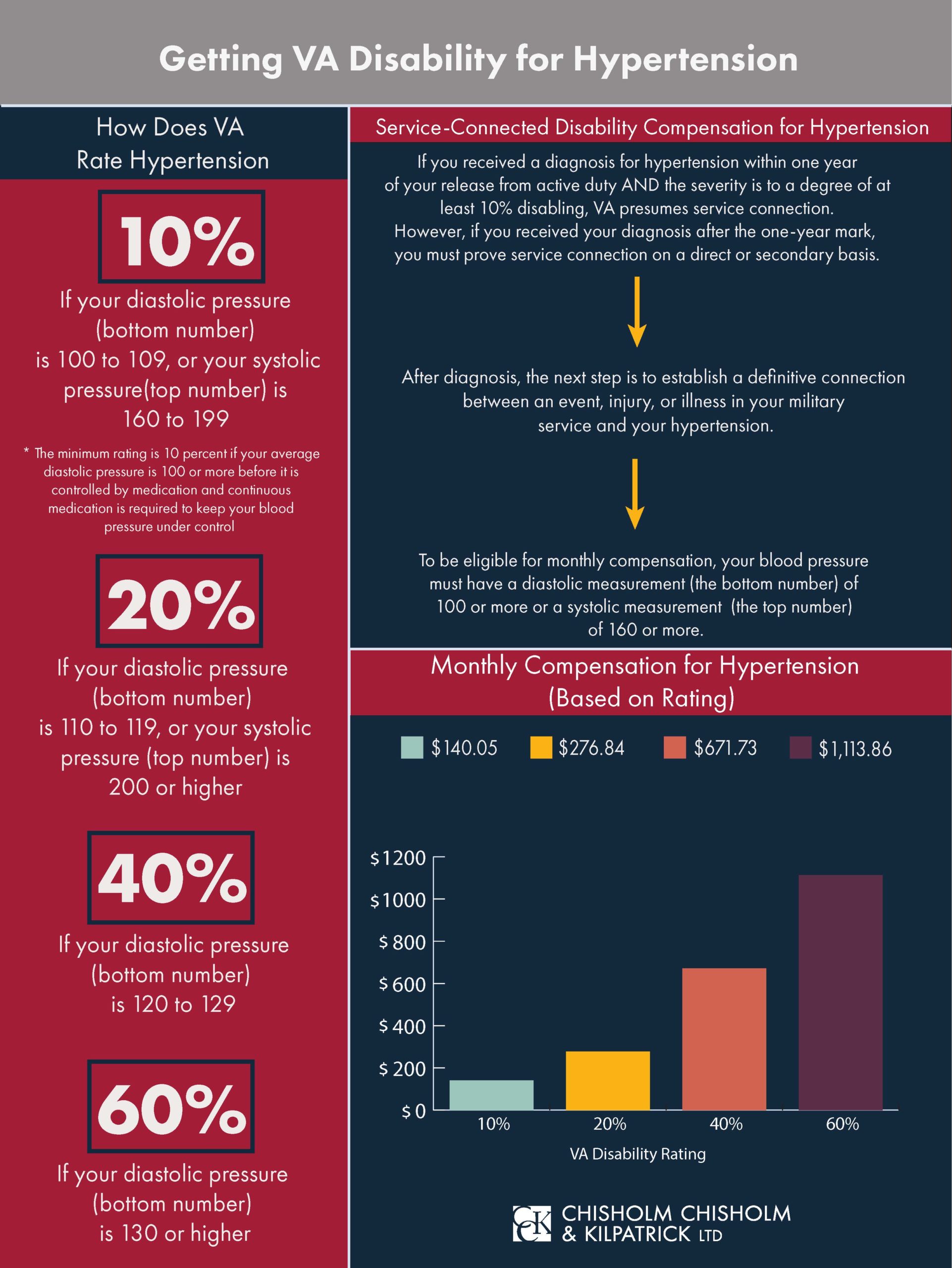
However, VA defines hypertension as 90 or higher for diastolic and 160 or higher for systolic. VA ratings are given at 10, 20, 40, and 60 percent based on these numbers.
Hypertension usually has no warning signs or symptoms, and many people may be unaware that they have this condition. Essentially, taking your blood pressure is the only way to know whether you have high blood pressure.
Hypertension is usually caused by unhealthy lifestyle choices, such as not getting enough regular physical activity and exercise. However, other health conditions, including diabetes and obesity, can also cause or increase the likelihood of hypertension.
In some cases, people with hypertension can lower their blood pressure into a healthy range by making lifestyle changes (e.g., getting 150 minutes of physical activity each week, not smoking, eating a healthy diet with limited sodium and alcohol, keeping a healthy weight, managing stress).
On the other hand, some people need to take medicine to manage their blood pressure. Examples of medications for hypertension include thiazide diuretics, angiotensin-converting enzyme (ACE) inhibitors, and calcium channel blockers.
How VA Rates Hypertension
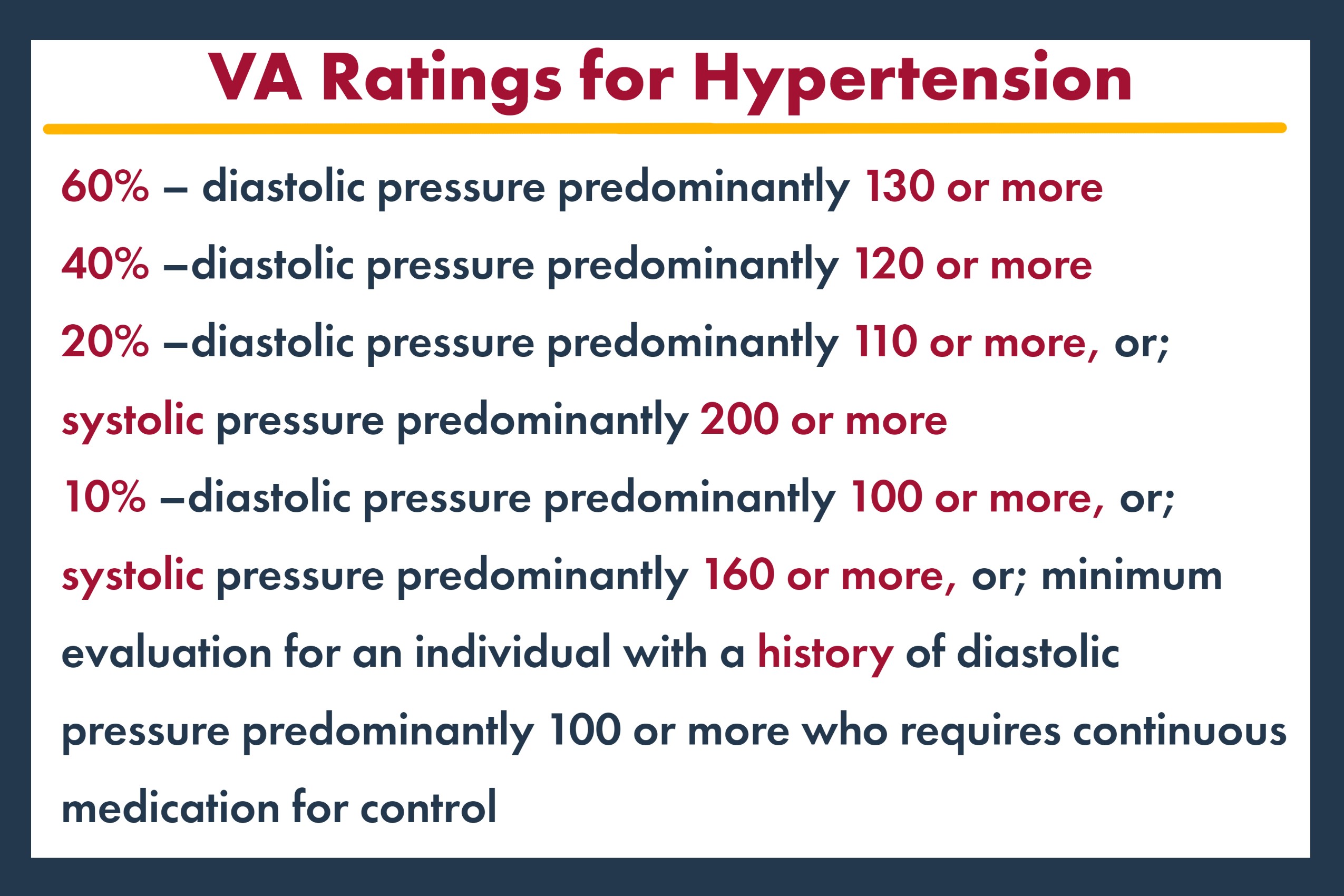
VA rates hypertension the same whether service connection is established directly, presumptively, or secondarily due to sleep apnea. Specifically, VA uses 38 CFR § 4.104 – Schedule of Ratings, Cardiovascular System, Diagnostic Code 7101. The rating criteria are as follows:
- 60% – diastolic pressure predominantly 130 or more
- 40% –diastolic pressure predominantly 120 or more
- 20% –diastolic pressure predominantly 110 or more, or; systolic pressure predominantly 200 or more
- 10% –diastolic pressure predominantly 100 or more, or; systolic pressure predominantly 160 or more, or; minimum evaluation for an individual with a history of diastolic pressure predominantly 100 or more who requires continuous medication for control
What is Sleep Apnea?
Sleep apnea is a potentially serious sleep disorder in which a person’s breathing is repeatedly interrupted during the course of the night. There are three main types of sleep apnea, including the following:
- Obstructive Sleep Apnea – the most common form of sleep apnea; occurs when the throat muscles intermittently relax and block your airway during sleep
- Central Sleep Apnea –occurs when your brain does not send the proper signals to the muscles that control breathing
- Complex (Mixed) Sleep Apnea Syndrome –occurs when someone has both obstructive sleep apnea and central sleep apnea
Signs and Symptoms of Sleep Apnea
The signs and symptoms of these three types of sleep apnea tend to overlap, sometimes making it difficult to determine which type you have. Symptoms can include:
- Loud snoring
- Gasping for air during sleep
- Awakening with a dry mouth
- Morning headache
- Hypersomnolence, or excessive daytime sleepiness
- Difficulty concentrating
Diagnosing Sleep Apnea
To confirm a sleep apnea diagnosis for VA disability compensation purposes, VA requires that a sleep study be conducted.
If you have previously been diagnosed with sleep apnea, but have not undergone a sleep study, VA will not consider that diagnosis enough evidence to verify eligibility for compensation.
VA may then rate the condition at 0, 30, 50, or 100 percent, depending on severity.
Treating Sleep Apnea
For mild cases of sleep apnea, doctors may suggest lifestyle changes such as losing weight or quitting smoking, if applicable.
In more serious cases, doctors may prescribe the use of a continuous positive airway pressure (CPAP) machine. A CPAP machine delivers air pressure through a mask while you sleep that is somewhat greater than that of the surrounding air. This allows your upper airway passages to remain open, thereby preventing apnea and snoring.
Service Connection and VA Ratings for Sleep Apnea
To establish service connection for sleep apnea on a direct basis, veterans must show evidence of the following:
- A current diagnosis of sleep apnea, as confirmed by a sleep study;
- An in-service event, injury, or illness; and
- A medical nexus (i.e., link) between their sleep apnea and the in-service event, injury, or illness
Once service connection is awarded, sleep apnea is then rated under 38 CFR § 4.97, Diagnostic Code 6847 – Sleep Apnea Syndromes (obstructive, central, mixed). Veterans are assigned a 0, 30, 50, or 100 percent rating depending on the severity of their condition. The rating criteria are as follows:
- 100% – chronic respiratory failure with carbon dioxide retention, the need for a tracheostomy, or cor pulmonale (i.e., the enlargement or failure of the right side of the heart due to lung disease)
- 50% – if a veteran requires the use of a breathing assistance device, such as a CPAP machine
- 30% – the veteran is experiencing persistent daytime hypersomnolence (i.e., a condition characterized by chronic daytime sleepiness that does not improve even with sufficient sleep)
- 0% – if the veteran’s condition is asymptomatic (i.e., condition that is not producing symptoms) but has a documented sleep disorder
Relationship Between Hypertension and Sleep Apnea
According to the American Heart Association journals and other research, obstructive sleep apnea is highly relevant to patients with hypertension.
- An estimated 50 percent of patients with hypertension also have obstructive sleep apnea.
- Obstructive sleep apnea represents the most prevalent secondary contributor to hypertension.
- Another study found that people with untreated sleep apnea were 6 times more likely to experience cardiovascular complications, such as hypertension.
Researchers believe that when breathing is restricted, oxygen levels in the body decrease, thereby causing an increase in blood flow. Increased blood flow places additional pressure on the blood vessels’ walls, ultimately causing higher-than-normal blood pressure levels. Overall, there is a clear causal relationship between sleep apnea and the development of hypertension.
Forms of Service Connection for Hypertension
Direct Service Connection
Similar to sleep apnea claims, veterans must establish the following three elements when applying for direct service connection for hypertension: (1) a current diagnosis of hypertension; (2) evidence of an in-service event, injury, or illness; and (3) a medical nexus linking the diagnosis to the in-service occurrence. However, direct service connection is not the only way in which veterans can be compensated for hypertension. Instead, veterans may be eligible for service connection for hypertension on a presumptive or secondary basis as well.
Presumptive Service Connection
VA presumes certain conditions are related to veterans’ military service. In this case, service connection will be awarded without having to provide a medical nexus opinion. For hypertension, VA presumes service connection if veterans receive a diagnosis within one year of discharge from military service and the condition is rated at least 10 percent disabling.
Secondary Service Connection
A secondary service-connected condition is one that results from a condition that is already service-connected. In claims for secondary service connection, proving a medical nexus is especially important. With regard to the conditions discussed herein, veterans may be eligible for service connection on a secondary basis for hypertension as due to sleep apnea. That is, if a veteran is service-connected for sleep apnea and later develops hypertension, they should subsequently be service-connected for hypertension based on the medical evidence outlined above.
To apply for secondary service connection for hypertension, veterans can file a claim the same way they would file an initial claim for service-connected compensation.
How to Prove Hypertension Secondary to Sleep Apnea
To establish a nexus between your already service-connected sleep apnea and your hypertension, you will need to submit evidence proving the link between your two conditions.
Specifically, you will need to demonstrate two things to VA to be granted service connection for a secondary condition:
- A diagnosis for your secondary condition; and
- Medical evidence showing the link between your service-connected condition and secondary condition.
Types of Evidence to Submit to Help Prove the Connection
- Doctor’s Note, or Medical Nexus—It can be helpful to have a doctor submit a letter stating that there is a causal relationship between your sleep apnea and your hypertension. Your doctor should state that they believe your hypertension is at least as likely as not caused by your sleep apnea.
- Relevant Medical Records—Relevant medical records can help show the connection between the two conditions and prove that your hypertension is linked to your sleep apnea.
- Medical Articles—Articles written for medical journals or other reputable sources can serve as evidence to support the causal relationship between sleep apnea and hypertension.
- Lay Evidence—Lay evidence refers to statements that are written by the veteran, the veteran’s family, or fellow service members, which speak to the veteran’s medical conditions or their service. Lay evidence can help support a claim for hypertension secondary to sleep apnea, as the veteran can speak to their experience with both conditions. Importantly, however, the person writing lay evidence should only speak to what they know. This means that the veteran cannot necessarily submit a medical opinion saying that their sleep apnea directly caused their hypertension, but they can speak to how both conditions affect them.
Was Your VA Disability Claim Denied?
The veterans’ benefits attorneys and advocates have decades of experience successfully representing veterans and their families before the Department of Veterans Affairs, the Court of Appeals for Veterans Claims, and the Federal Circuit. If your VA claim has been denied, we may be able to help. Contact us today at 800-544-9144.
About the Author
Share this Post