What is long-term disability insurance?
Long-term disability (LTD) insurance replaces all or a percentage of a person’s income if they are unable to work due to sickness or injury. It can be purchased directly from an insurance company or received as an employment benefit. Each LTD policy is different and has specific requirements that must be met before benefits are paid, so it is important to read your policy carefully to understand your coverage, the policy’s terms, and any benefit limitations.
What information is in a long-term disability policy?
Although the specific provisions vary from policy to policy, there are some important categories of information that appear in all long-term disability policies. First, your LTD policy will tell you what definition of disability you need to meet in order to receive benefits. Second, your LTD policy will provide information about your benefits, including when your benefits will start, what your monthly benefit will be, and how long you can receive benefits. Third, your LTD policy will tell you what limitations, if any, apply to benefits under that policy. Benefit limitations can prevent you from receiving benefits or restrict the amount of time you can receive them for. Common LTD policy limitations include preexisting condition limitations, mental health limitations, and appropriate care and treatment limitations.

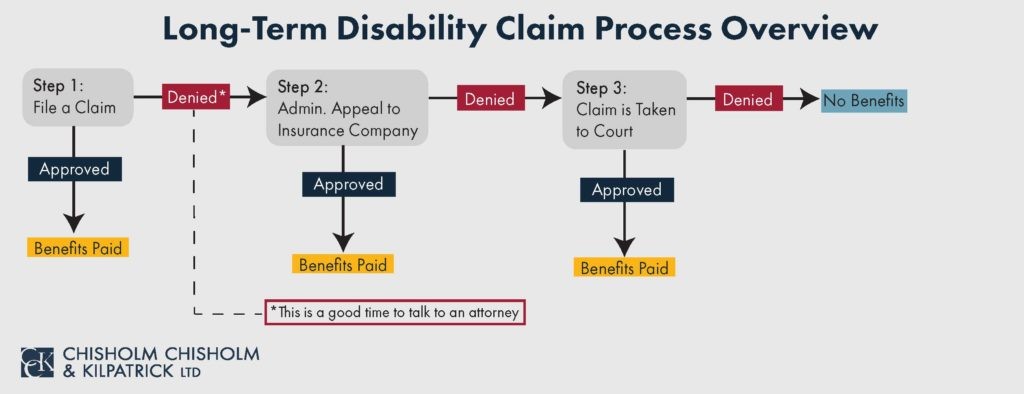
What does the long-term disability claim process usually look like?
The long-term disability claim process has three main stages: 1. The initial claim; 2. The administrative appeal; and 3. Litigation in court.
Long-Term Disability Initial Claim
To initiate a long-term disability claim, you must submit notice of claim to the insurance company, in accordance with the policy’s instructions for doing so. After you submit notice of claim, the insurance company will ask you and your treating physicians to complete claim forms. You also need to collect and submit evidence of your disability. Although the primary source of evidence should be your medical records, it can also include reports from your treating doctors, photos, symptom logs, or statements from yourself, your family and friends, or your coworkers. After you have submitted your claim forms and evidence of your disability, the insurance company will investigate to determine whether you are entitled to benefits and then either approve or deny the claim. If your claim is approved, you will start to receive long-term disability benefits and the insurance company will periodically conduct claim updates to determine if you continue to meet the applicable definition of disability. If your claim is denied, then you move on to the next stage of the claim process – the administrative appeal.
Long-Term Disability Administrative Appeal
Your administrative appeal should address the insurance company’s basis for the claim denial. It should explain why the insurance company’s decision was wrong and provide supporting evidence. The appeal is a critical stage in the long-term disability claim process because it is often your last opportunity to get evidence into the record. If evidence is not submitted with your appeal, you likely will not be able to submit it later in court. Additionally, if you do not appeal, or appeal after the deadline to do so has already passed, you may lose your rights to your LTD benefits completely. Given the importance of the administrative appeal, it is a good time to consider consulting with a long-term disability attorney.
Long-Term Disability Litigation in Court
If the insurance company denies your appeal, then you move on to the third, and final, stage of the claim process – litigation in court. Litigation of LTD benefits under employer-provided group policies is unique. Such claims are governed by federal law, the Employee Retirement Income Security Act (ERISA). There is no jury in these cases and, as mentioned above, the evidence is largely limited to the insurance company’s claim file. Further, the court may give deference to the insurance company’s decision to deny benefits. Even if the claimant is successful in court, the remedies are limited in ERISA-governed cases.
What is ERISA?
Although there are exceptions, most disability, life, health and long-term care policies, as well as pension benefits, provided by your employer are covered by the Employee Retirement Income Security Act (ERISA). This federal statute usually pre-empts state laws designed to protect consumers and creates significant (but not insurmountable) hurdles for claimants seeking benefits to which they were promised. Our lawyers know how to interpret these ERISA statutes, the applicable Department of Labor Regulations, the plan documents and the case law of the federal courts to protect your entitlement to benefits.
If you purchased a long-term disability, short-term disability, life insurance, long-term care insurance policy or you work for the government or a church-related organization, then ERISA does not usually apply and the state laws designed to protect insured individuals are available for our attorneys to use in securing your benefits. Regardless of the specific type of policy you have, we will work to secure your benefits.
If your claim has been denied, you may have a limited amount of time to appeal the decision, so it is important to get help as soon as possible.
Everything ERISA: Blogs, Videos, and More.
Join the Discussion:






ERISA Law
Can You Receive Long-Term Disability Benefits After Suffering a Catastrophic Injury?
February 18, 2025




ERISA Law
Witness Statements: What They Are and How They Help with Long-Term Disability Claims
December 4, 2024

CCK Gets Results
Hear from a CCK client
CCK Covers the Nation
Chisholm Chisholm & Kilpatrick LTD assists individuals with claims and appeals across the nation. Learn more about the services we offer in your home state.