Long-Term Disability Waiting Period: What to Expect

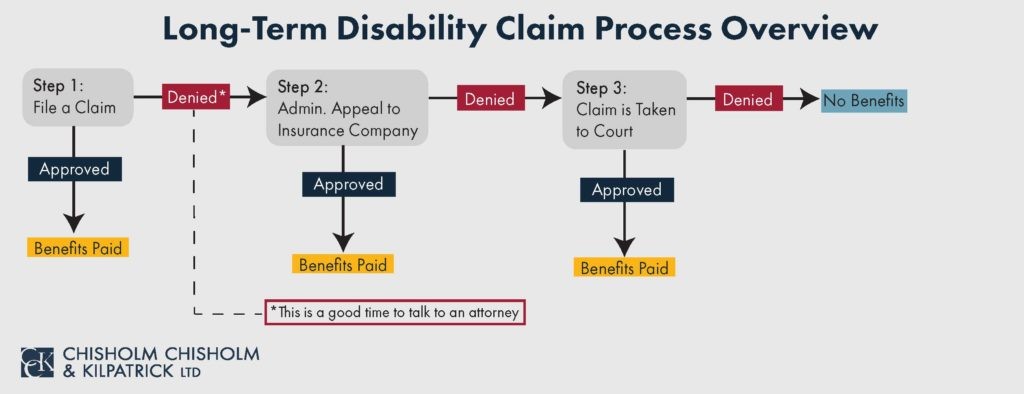
Obtaining long-term disability benefits is often challenging. Insurance companies, such as Humana or New York Life, deny disability claims often. Moreover, these policies also include a waiting period during which you are unable to receive benefits. It is important to thoroughly read your policy to know exactly how long this period lasts so that you can prepare for it.
This article will discuss what the waiting period (or elimination period) is and what LTD claimants can do during this period when they cannot work but still need benefits.
What is the Waiting Period?
If you become unable to work and file a long-term disability (LTD) claim, then the insurance company does not immediately start paying benefits. In order to qualify for long-term disability (LTD) benefits, you typically must meet the definition of disability for 90 – 180 days before the insurance company will begin paying benefits. This is typically known as the waiting period or elimination period. In employer-provided policies, the waiting period may vary for different classes of employees covered by your policy.
You should read your policy carefully to ensure you understand the definition of disability you need to meet and how long your waiting period is. You may be denied benefits if you fail to meet the definition at any point during the waiting period. Reading your policy and understanding it can sometimes be confusing and time-consuming. You should consider contacting an attorney if you are unsure what your policy provides.
The Definition of Disability During the Waiting Period
As mentioned, you must continue to meet your policy’s definition of disability during the waiting period. There are two types of definitions that your insurance policy may contain: “own occupation” or “any occupation.” In short, own occupation definitions ask claimants whether they can perform the occupational duties of their own job, but an any occupation definition asks whether claimants can perform the duties of any job whatsoever.
Therefore, if your insurer finds you disabled under the “any occupation” definition, then you must still be disabled under this definition when the waiting period concludes. Of course, this period can be stressful for LTD claimants since during this period, though they may remain disabled and unable to work, they cannot receive benefits.
What Do I Do During the Long-Term Disability Waiting Period If I Cannot Work?
If their employer provides it, many people will collect short-term disability (STD) benefits during the long-term disability waiting period. The waiting period for short-term disability benefits is usually only 7 to 14 days, making it a good source of income shortly after you become disabled. Typically, for those who have both short-term and long-term disability insurance coverage, STD benefits will last for the entire long-term disability waiting period.

At that point, it is common for people to then transition to long-term disability benefits. However, it is important to note that you may have your LTD claim with one insurance company and your STD claim with another. It is generally easier to transition from short-term disability to long-term disability when the same insurance company administers the policies.
Alternatively, you may have state-provided disability insurance that you were paying into while you were working. For example, you may have Rhode Island has Temporary Disability Insurance if you are a Rhode Island employee who is unable to work. This benefit can help supplement your income during the long-term disability waiting period. These benefits are usually accessible quickly with supporting medical reports or records. You should check to see if these benefits are available to you through your state.
Contact the Long-Term Disability Attorneys at CCK
At Chisholm Chisholm & Kilpatrick LTD, our team of experienced attorneys and professionals can assist you with your long-term disability claim. We understand that disability policies are confusing and insurance companies don’t always appear to act in their insureds’ best interest. Call CCK today at (800) 544-9144 for a free case evaluation to see if we can help you get the benefits to which you are entitled.
About the Author
Share this Post
