Getting Long-Term Disability (LTD) Benefits for COVID-Related Symptoms

The COVID-19 global pandemic has introduced new challenges to many across the world. Some studies estimate that more than 40 percent of those who have survived COVID-19 have (or had) long-term COVID-related symptoms. People with long COVID, a.k.a., “COVID long haulers,” have symptoms associated with this illness that linger for months and months, even after the virus has left the body.
Consequently, many who suffer from COVID-related symptoms find it impossible to work. When a person finds that their ability to work is impaired, they must consider filing for long-term disability (LTD) benefits. Yet receiving LTD benefits for COVID-related symptoms is very difficult as the virus has only been around since December of 2019.
The long-term disability lawyers at Chisholm Chisholm & Kilpatrick understand how difficult this is for claimants and want to help. Regardless of whether you are filing an initial claim or appealing a denial of benefits, we can ease the burden. Call us today at (800) 544-9144 for a free consultation with a member of our team.
What Are COVID-Related Symptoms?
Notwithstanding that many people who get COVID-19 can go back to work, there are many who cannot. The symptoms associated with long-term COVID can be new or ongoing. Moreover, some of these symptoms may not begin until the virus itself is out of your body.
COVID-related symptoms can include:
- Tiredness and/or fatigue;
- Concentration issues;
- Depression and/or anxiety;
- Difficulty thinking (i.e., brain fog);
- Shortness of breath;
- Chest pain;
- Headaches;
- Heart palpitations;
- Muscular and joint pains;
- Dizziness;
- Coughing;
- Fever; or
- A loss of taste and/or smell.
Additionally, there can be physical damage to certain organs within the body, such as the heart, lungs, or brain.
How Can COVID-Related Symptoms Impair a Person’s Ability to Work?
Regardless of what job you have, adequately performing the duties thereof when you suffer from COVID-related symptoms can seem like an impossible task. COVID-related symptoms can greatly disrupt a person’s life. Consider “shortness of breath” when trying to do your job; when you have difficulty breathing it can put a stop to whatever you are doing. Likewise, if you routinely get dizzy or are fatigued, your cognitive and physical abilities are weakened.

It is evident how these symptoms can make working difficult. Take a traveling business consultant as an example. A traveling business consultant travels from office to office—sometimes in different states across the country—offering top-level advice and solutions for businesses. What if this consultant gets dizzy frequently or has difficulty thinking and remembering small details? Conducting an important business meeting can become strenuous, and the consultant most likely will have to excuse themselves.
Moreover, when a person has suffered from COVID, they may also develop other complications, such as chronic kidney disease or chronic fatigue syndrome. A brain surgeon, for example, who experiences fatigue and concentration issues is likely to make mistakes, but a mistake in this profession can have dire consequences. It is sometimes not only the health of the professional at risk but also the risk of their patients.
Nevertheless, it is evident how the lingering symptoms of COVID can sideline a person and cause them to seek out long-term disability benefits. For many, it seems like the best option. What is known as long COVID is now considered a disability, but it can still be difficult for people to receive approval from their insurance company.
Why Is It Difficult to Receive Long-Term Disability Benefits for COVID-Related Symptoms?
Long COVID is a new medical condition about which scientists are still learning. As such, there are still many question marks when it comes to its long-term effects. This does not change how it impacts a person’s ability to work, however. It may still qualify for long-term disability insurance benefits.
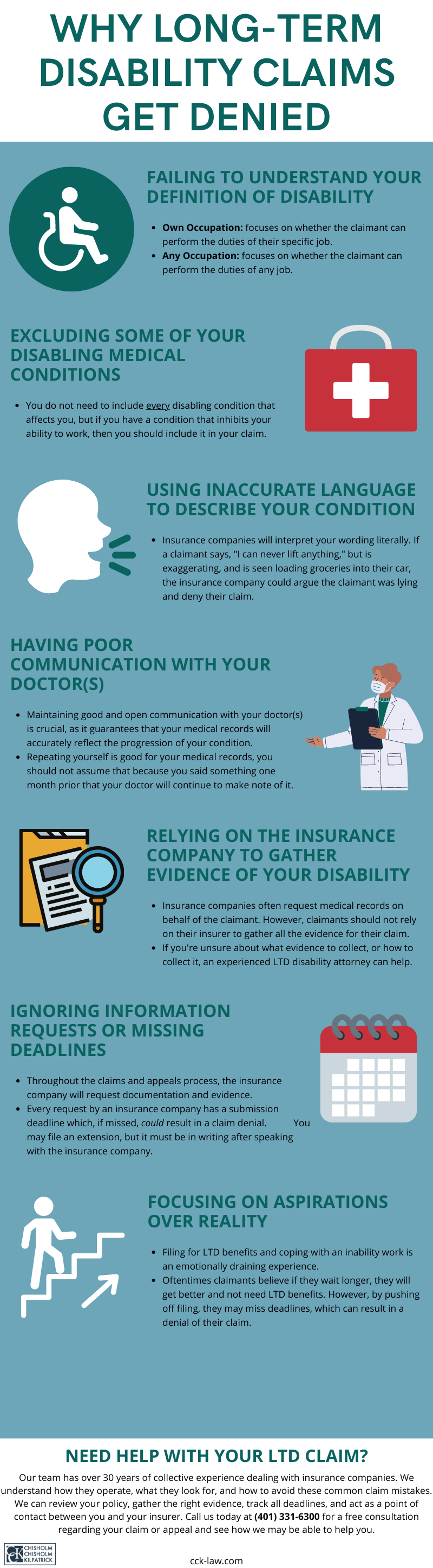
Yet why do so many insurance companies issue long-term disability claim denials for COVID-related symptoms quite frequently? While claimants will experience many of the above-mentioned symptoms, certain tests will not show that anything is wrong with them. Insurance companies prefer objective evidence over self-reported symptoms.
For example, a person suffering from COVID-related symptoms will have clean X-rays, EKGs, and other tests that are normally submitted as part of a claim. An insurance company is likely to point to these tests and claim that since they came out “clean” there is no reason for disability benefits.
Moreover, insurance companies will routinely deny these types of claims because claimants can still perform sedentary duties related to other jobs. It is important to remember that insurance companies do not like paying claims if they can help it. Therefore, these companies will try and find any reason to issue a denial of benefits, regardless of the disability in question.
While many claimants have been denied long-term disability benefits due to symptoms related to the coronavirus, many have received approvals for both short- and long-term disability benefits.
Filing an LTD Claim for COVID-Related Symptoms
To receive LTD benefits, you must prove that you are disabled per the definition of disability located within your policy. All policies have this definition of disability, and it typically contains one of two definitions: own occupation and any occupation.
The own occupation definition of disability asks whether you can perform the duties of your specific job, while the any occupation definition of disability asks whether you can perform the duties of any job whatsoever.
As is evident, the any occupation definition is much harder to prove. For example, if you are a heart surgeon and have a medical condition that prevents you from handling surgical tools, but you can still work at a computer, then your insurance company could deny your claim.
Unfortunately, COVID-related symptoms can be difficult to prove for disability purposes. It is vital that you receive an official diagnosis of long COVID to show the origin of the symptoms that are preventing you from working.
However, medical records are not always sufficient to win a claim by themselves. It is crucial to submit supplemental evidence as part of your claim. This supplemental evidence is an opportunity to show how your COVID-related symptoms impact your ability to work.
How Can Chisholm Chisholm & Kilpatrick Help with Getting LTD Benefits?
The legal team at Chisholm Chisholm & Kilpatrick understands the difficulties of obtaining long-term disability benefits when suffering from symptoms related to the coronavirus. While these claims can be difficult, this is not a process you must go through alone. The long-term disability lawyers at CCK are ready to assist you.

Our team will thoroughly evaluate your LTD policy. We will make note of the definition of disability located therein and determine the best evidence to gather to prove your claim. Moreover, we will help gather this evidence so that you may focus on managing your health.
Insurance companies are very difficult to work with when it comes to LTD benefits, and this is especially true when your disability is related to COVID. However, our experienced attorneys have over three decades of collective experience dealing with insurance companies and know how they operate. We will act as a point of contact so that you do not have to deal directly with them.
Supplemental evidence is a very important part of an LTD claim for COVID-related symptoms. CCK works with a variety of outside experts that can provide evaluations of your condition. A vocational evaluation, for example, can show how your condition impacts your ability to do your specific job.
Additionally, if your policy is provided by your employer, an ERISA attorney can help you navigate the claim process. Group policies are ERISA governed and come with their own strict deadlines and rules. We will track all documentation, evidence, and deadlines to ensure that it is submitted on time.
Call CCK Today for a Free Consultation
At CCK, we understand that suffering from COVID-related symptoms is a stressful experience that may seem impossible to overcome. It is a new problem that many are facing. We want to help you navigate this process so that you may receive the benefits you deserve.
Call us today at (800) 544-9144 for a free consultation with a member of our team and see how we may be able to help you.
Share this Post