Aetna Long-Term Disability Denial: How to Appeal
Aetna is an American health care company that offers insurance such as disability, medical, dental, pharmaceutical, and behavioral health care, in addition to other health benefit programs. Aetna was born out of a fire insurance company in the early 19th century, its name was inspired by the most active volcano in Europe at the time, Mt. Etna. Over time, Aetna split from its fire insurance counterpart and became a life insurance company, and eventually began to offer health coverage, becoming a major American provider.
If you have a disabling health condition and are unable to work, you may be covered by a long-term disability plan from Aetna. If approved, long-term disability insurance will cover a percentage of your work income. While Aetna has been deemed one of the best health insurance companies in 2021, it is common for even highly rated insurance companies to make filing an insurance claim difficult.
The long-term disability process can be challenging, and companies like Aetna frequently deny claims. An Oklahoma case in 2018 highlighted an instance in which Aetna’s medical directors did not thoroughly evaluate a woman’s cancer claim before denying her treatment.
If your long-term disability claim has been denied by Aetna and you are filing an appeal, there are steps you can take to strengthen your claim. It can benefit you to contact an experienced long-term disability attorney to aid you in the appeal process, which can grow complicated. The long-term disability lawyers at Chisholm Chisholm & Kilpatrick have experience handling appeals from companies such as Aetna. You can contact us at 800-544-9144 for a free complimentary consultation.
Why Aetna May Have Denied Your Claim
If your claim was denied by Aetna, you likely received a letter by mail explaining the reasons behind the denial. You will want to make sure that you carefully review this letter and make sure that you understand why your benefits were denied. By recognizing the ways your claim lacked strength, you can pinpoint these weak spots and reinforce them with evidence in your appeal. Your denial letter will likely also include instructions on how to move forward in the appeal process.

Unfortunately, there are many reasons why Aetna may deny your claim. You may need stronger evidence, or the definition of disability in your claim was not satisfied. Aetna may also use surveillance tactics on you to find specific activities from your daily life that they can use to deny your claim. Other times, such as in Aetna’s 2018 Oklahoma case of bad faith, it could even be lack of diligence on the insurance company’s part.
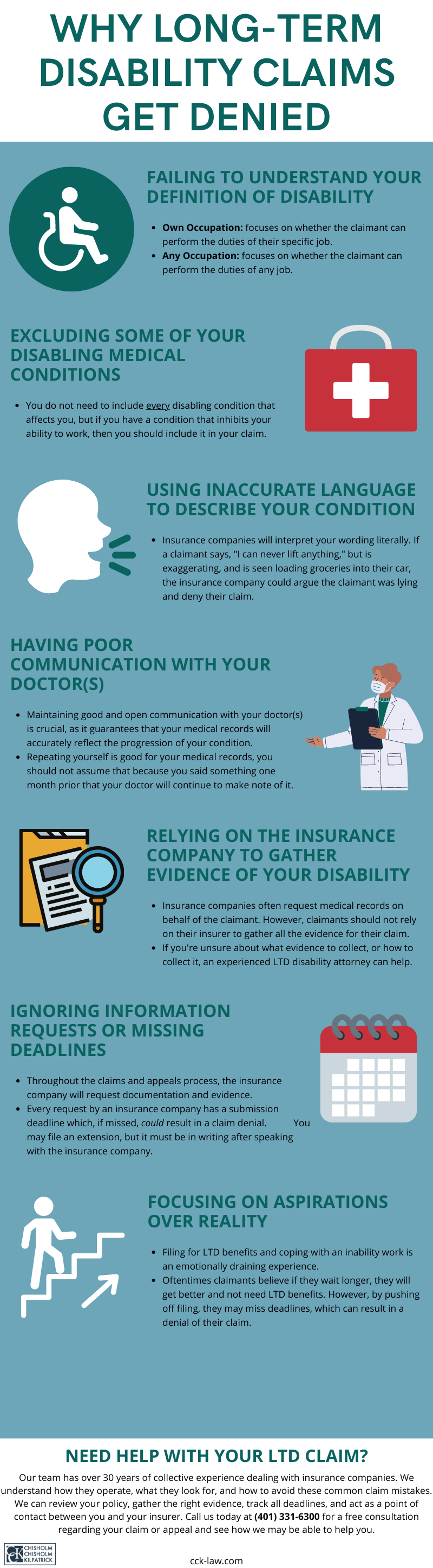
Other reasons Aetna could deny your claim include:
- You did not satisfy your definition of disability: One of the most crucial parts of your long-term disability claim is meeting the definition of disability outlined in your policy. This policy is what determines if your condition warrants benefits. Your definition of disability may either be the own occupation definition, which means you must be disabled from working your specific job, or the any occupation definition, which means you must be disabled from working any occupation in the workforce.
- You want to make sure that the evidence you provide proves your specific definition. It is also important to note that the definition can change over time. A claim may initially require you to meet the own occupation definition and then transition to the any occupation definition. It is important to be aware that you may have to provide new evidence during this transition to avoid further denial.
- Insufficient evidence: Medical evidence is necessary for long-term disability claims, beginning with your medical records. However, medical records alone are often not enough to satisfy your definition of disability. If you were denied benefits because you did not submit enough evidence, you can seek further evaluations by additional medical experts or consult a vocational expert. They may be able to provide additional assessments of your condition or your abilities to perform your work duties while disabled.
- Aetna’s own experts evaluate you: Aetna may use its own experts to compile evidence for your claim. This can be dangerous, as these hired professionals may be biased toward Aetna. They may not fairly evaluate your impairment, which can hurt your claim or increase your chances of being denied. Seeking evidence from trusted physicians and outside experts can help you gain evidence that can combat these biased evaluations.
- Surveillance tactics: It is not uncommon for insurance companies to hire private investigators to watch you with the intention of catching you at an activity that may disprove your disability. Investigators may perform stakeouts, record videos, photograph you, and screen your social media. Representatives from Aetna may even make house calls in order to observe you. If anything is found that Aetna believes disproves your disability, they may use that as a reason to deny your claim.
- For example, you are caught on camera lifting a bag of groceries when your claim says you cannot lift heavy objects. To refute this in your claim you will want to be as specific about your abilities as possible. Maybe you cannot lift 15 pounds, but you can lift less than that, which might include a small bag of groceries.
How to Appeal a Long-Term Disability Denial from Aetna
In your appeal for long-term disability benefits, you want to make sure that you build a case that fights the reasons listed in your denial letter. The evidence you submit in your appeal is crucial, especially if your long-term disability plan is governed by ERISA law. Under ERISA, the appeal is your last chance to introduce new evidence. If your case is denied again and taken to court, you will no longer be able to submit further evidence for your claim.

Regardless, you likely want your claim approved sooner rather than later, and it is important to make sure you get the right kinds of evidence on your record. Steps that can be taken in your appeal include:
- Request a report from your treating physician: Medical records do not always cover the full scope of your condition. A written report from your physician may be able to highlight certain aspects of your illness overlooked in your medical records. It is crucial to maintain an honest relationship about your condition with your physician, so that they may be able to fully detail the aspects of your condition in their letter.
- Impact statements from friends, family, and coworkers: Personal acquaintances have likely seen the ways your condition affects your life. They may be able to provide statements that can demonstrate how they have witnessed your illness impact your daily activities. Friends or family may be able to speak to specific instances in which your condition has affected your home or personal life, while coworkers can provide evidence for how it hinders your work life or job performance.
- Expert opinions: Opinions and evaluations from experts, in addition to your regular physician, can be important supplementary evidence to your claim. Medical experts may be able to provide functional capacity or neuropsychological exams. Vocational experts may be able to assess your occupation, or all occupations in the workforce, and your ability to be able to perform job duties with your condition. Additional assessments can be a strengthening asset to your claim.
- Fix any errors in your initial claim: It is possible that your claim was denied because your initial application contained errors or missed certain information or deadlines. The appeal is your chance to correct your claim, fix any errors in information, and ensure that all requirements and deadlines are met. It is important to study your policy carefully to ensure you are following all of Aetna’s guidelines.
Chisholm Chisholm & Kilpatrick Can Help You with Your Long-Term Disability Appeal
It is possible for you to handle your appeal with Aetna on your own, but there are benefits to seeking the help of an attorney for your long-term disability appeal. An experienced long-term disability lawyer, such as those at CCK, can advise you on the steps you need to take to submit a strong appeal. We can lift a significant portion of the legal burden off of you so that you are able to focus on managing your health.

Our long-term disability lawyers will assess your policy, keep track of deadlines, and can handle the communication between yourself and Aetna, as well as your doctors. We will make sure that you are submitting the strongest claim possible, and know-how to proceed if any bad faith is suspected on Aetna’s part. We understand how insurance companies often prioritize their own business interests over the needs of claimants and can ensure that your claim is being treated fairly.
We understand that filing an appeal can be strenuous, especially after you have already dealt with the stress of a denial. Our legal team wants to make this process as stress-free as possible for you. After you are approved, we can continue to help you provide any requests for updated information Aetna may require. We want you to be able to receive the benefits you deserve.
Contact the Attorneys at Chisholm Chisholm & Kilpatrick LTD for a Free Consultation
The long-term disability team at Chisholm Chisholm & Kilpatrick has the knowledge you need to help with your appeal against Aetna. We have over three decades of collective experience fighting for long-term disability benefits. If you have a condition that disables you to the point that you are no longer able to work, you can speak with a member of our team at 800-544-9144 or contact us online at no cost to you.
Share this Post