VA Ratings for TBI with Migraines
CCK Law: Our Vital Role in Veterans Law
What is a Traumatic Brain Injury (TBI)?
Traumatic brain injury (TBI) is an injury to the brain that often occurs as the result of a blow to the head or an object penetrating the brain. TBI can result in brain dysfunction and other serious issues.
Military service can place servicemembers at a higher risk for TBI than civilians. Common occurrences of traumatic brain injury in the military can include:
- Combat exposure
- Motor vehicle accidents
- Personal assault
- Falls
Additionally, TBIs are considered a signature wound of the post-9/11 wars. This is likely due to the increased use of Improvised Explosive Devices (IEDs) during these wars.
A concussion, for example, is a common form of TBI; however, not all TBIs are concussions.
Diagnosing TBI
Diagnosing a traumatic brain injury can usually be done through the manifestation of symptoms. The following symptoms may begin to manifest cognitively, physically, behaviorally, and/or emotionally after a head injury:
- Impaired vision or hearing loss (e.g., tinnitus)
- Dizziness and headaches
- Weak muscles
- Stroke, seizures, or paralysis
- Coordination, balance, and gait disorders
- Difficulty with written and verbal communication
- Impaired memory and difficulty concentrating
- Depression
- Poor judgement
TBIs are initially diagnosed as mild, moderate, or severe based upon medical testing and the severity of the veteran’s symptoms. While mild brain injuries usually resolve themselves within about six months, there can be significant residuals associated with more severe cases.
How is TBI Rated?
VA rates traumatic brain injuries based on the residual symptoms a veteran is currently experiencing because of the trauma under 38 CFR § 4.124a.
Specifically, there are three main areas of dysfunction that can result from a TBI and affect a person’s ability to function: cognitive, emotional/behavioral, and physical. Residuals generally fall into these categories.
VA rates these residuals on a scale of 0, 1, 2, 3, or total, with each of these increments corresponding to a disability rating. Ratings can be given at 0, 10, 40, 70, or 100 percent.
TBI Presumptions
As of January 2014, VA presumes service connection for five diseases if precipitated by a service-connected TBI:
- Dementia
- Parkinson’s disease
- Seizures
- Depression
- Hormone deficiency
What Are Migraines?
Migraines are a form of intense headache that can last for many hours. There is no singular, definitive cause of migraines; however, triggers may include hormonal imbalance, alcohol use, stress, sensory stimulation, certain foods, and changes in environment. Typically, traumatic brain injury can cause recurring migraines.
Migraines can be characterized by the following symptoms:
- Nausea
- Vomiting
- Sensitivity to light and sound
- Lightheadedness
- Blurred vision
How Does VA Rate Migraines?
VA rates migraine headaches under 38 CFR § 4.124a, Schedule of Ratings – Neurological Conditions and Convulsive Disorders, Diagnostic Code 8100. This diagnostic code has ratings ranging from 0 to 50 percent, with criteria based on severity and frequency of the migraines. The rating assigned will correspond to the amount of VA disability compensation a veteran will receive. Below are the criteria for each rating:
- 50% – with very frequent completely prostrating and prolonged attacks productive of severe economic inadaptability
- 30% – with characteristic prostrating attacks occurring on an average of once a month over the last several months
- 10% – with characteristic prostrating attacks averaging one in two months over the last several months
- 0% – with less frequent attacks
The term “prostrating” generally means that the veteran’s migraine headaches are so severe and debilitating that they are required to lay down for an extended period of time due to complete exhaustion and physical weakness. Typically, prostrating migraines also require veterans to stop all activity and possibly take medication or seek medical attention.
How are Traumatic Brain Injury and Migraines Related?
Migraines are common in the general population; however, they may be even more prevalent among veterans. According to data published by VA, migraine diagnoses have “increased by 27 percent among all branches of the armed forces from 2001-2007.”
One possible cause for migraines among veterans is traumatic brain injury. Migraines that result from traumatic brain injury can sometimes be referred to as “post-traumatic headaches.” According to the American Migraine Foundation, other symptoms of TBI, such as sleep disorder, memory loss, dizziness, fatigue, and anxiety can make a veteran’s migraines worse.
Mild traumatic brain injuries are generally categorized by the loss of consciousness for less than 30 minutes following the injury. Data published by the American Migraine Foundation indicates that roughly 75 percent of mild TBIs come from blast injuries, while 29 percent come from falls and 22 percent from motor vehicle accidents. Due to the nature of service, veterans are at a higher risk of experiencing blasts, falls, and vehicle accidents than the average civilian. Additionally, blast exposures are “believed to heighten the risk of headaches and other symptoms.” After a TBI, headaches can take weeks or even months to develop.
Treatments for TBI with Migraines
Certain forms of medication may be used to treat TBI symptoms, such as migraines, and alleviate pain. Medications may include “non-steroidal anti-inflammatories for acute treatment or post-traumatic headaches and triptans for post-traumatic migraines”
How is TBI with Migraines Rated?
Typically, TBI is rated on the residuals meaning that a veteran will not receive a rating for both TBI and their symptoms of TBI, as this is considered pyramiding, or rating the same disability or symptoms of a disability twice.
However, migraines are one of the few exceptions to this rule, as a veteran can receive a rating for TBI and migraine headaches. This is because 38 CFR § 4.124a stipulates that any residual with a distinct diagnosis that can be evaluated under another diagnostic code may be given a rating separate from the rating assigned to residuals of TBI.
For example, a veteran may be rated at 70 percent for Traumatic Brain Injury residuals and have a 10 percent rating for migraines.
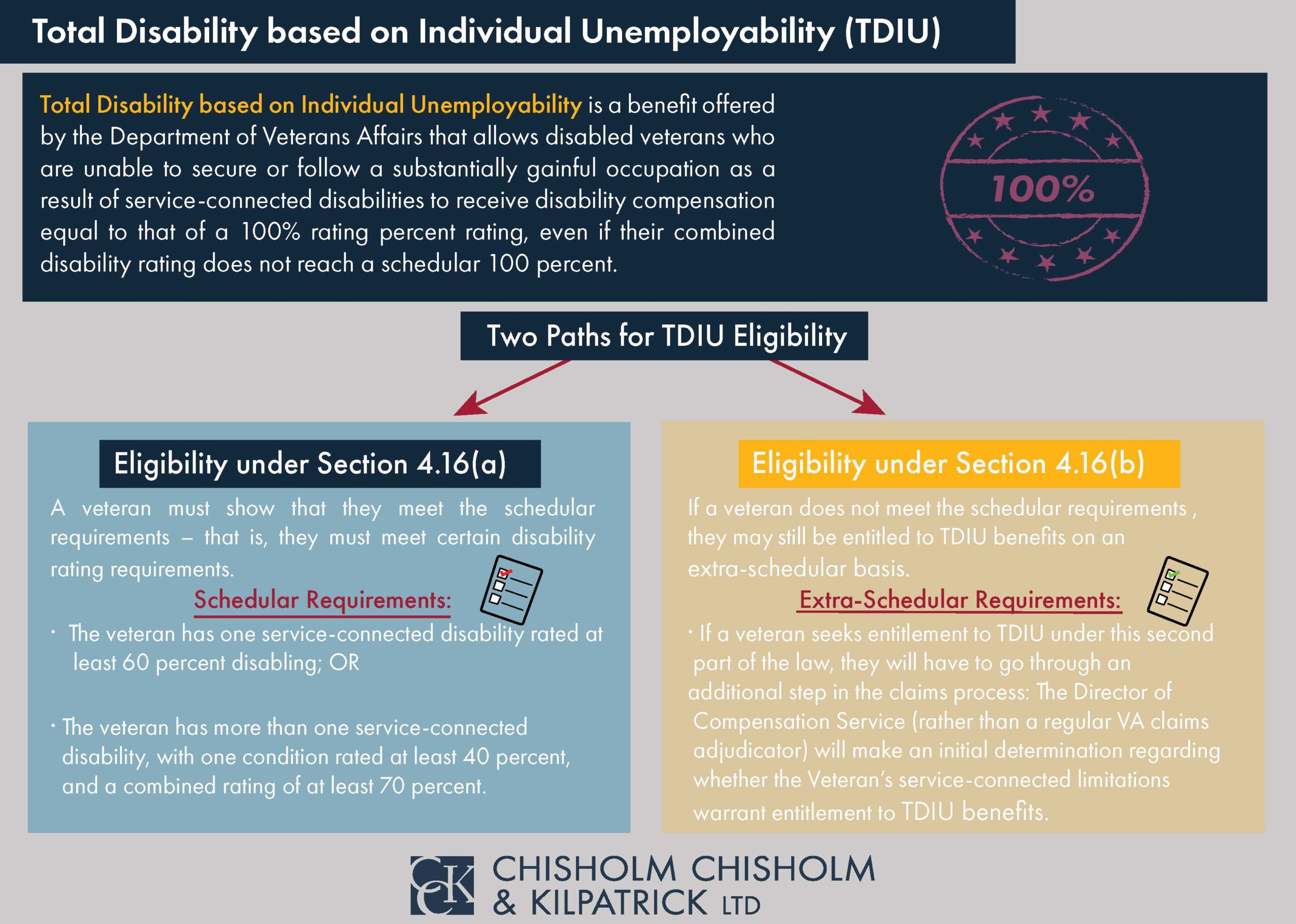
TDIU with TBI and Migraines
Veterans who have been unable to gain or obtain employment because of their service-connected brain injury and migraines may be eligible for TDIU.
TDIU, or total disability based on individual unemployability, is a monthly VA benefit that compensates veterans at the 100 percent level if they are prevented from working because of their conditions.
In order to be eligible for schedular TDIU, veterans must have one condition rated at 60 percent minimum OR two conditions that can be combined to reach 70 percent, where one condition is at minimum 40 percent. As such, secondary service connection can be extremely helpful in boosting veterans to the 70 percent minimum needed for multiple conditions to achieve TDIU. The criteria for schedular TDIU is outlined under 38 CFR § 4.16a.
Importantly, ratings for both migraines and TBI can contribute to a veteran’s eligibility for TDIU.
Veterans who do not meet the necessary criteria for schedular TDIU may be eligible for extraschedular TDIU. For this form of TDIU, veterans must prove that their condition(s) uniquely hinder their ability to maintain substantially gainful employment. Extraschedular TDIU is rated under 38 CFR § 4.16b.
Getting Assistance with Your TBI with Migraines Claim
If your claim for benefits for Traumatic Brain Injury has been denied, or if you have not been able to establish benefits for your migraines in addition to your TBI, the veterans’ advocates at Chisholm Chisholm & Kilpatrick may be able to help. Our experienced team can help build your appeal for TBI with migraines and submit documentation to VA on your behalf. Call us today for a free case evaluation.
About the Author
Share this Post