How to Prove VA Service Connection for Both Depression and Anxiety

CCK Law: Our Vital Role in Veterans Law
Veterans filing a claim for both depression and anxiety should be aware that VA generally does not assign separate ratings for the two conditions. Instead, VA treats nearly all mental health conditions under a single General Rating Formula for Mental Disorders in 38 C.F.R. § 4.130. This avoids prohibited “pyramiding” (rating the same symptoms twice) under 38 C.F.R. § 4.14.
That said, many veterans experience both depression and anxiety, and it is recommended to prove both for the most accurate mental health rating.
Key Points
- Depression and anxiety commonly share symptoms and are issued a single mental health rating.
- Separate ratings are only possible in exceedingly rare circumstances where completely distinct symptoms can be medically differentiated (e.g., a traumatic brain injury cognitive disorder versus PTSD), but depression versus anxiety almost never qualifies.
- However, providing evidence of both conditions can help ensure that VA gives the most accurate and maximized mental health rating.

How Do I Prove Service Connection for Both Depression and Anxiety?
The first step is to prove that both conditions are related to a veteran’s time in service. While there are several ways to show service connection, the two most common for depression and anxiety are direct service connection and secondary service connection.
Direct Service Connection: “Service caused my depression and anxiety.”
Generally speaking, there are three basic elements of service connection.
- First and foremost, veterans must have a current diagnosis of the condition (i.e., depression, anxiety).
- From there, veterans must show evidence of an in-service event, injury, or illness.
- Finally, veterans must provide a medical nexus linking the current, diagnosed condition to the in-service occurrence.
Importantly, in-service causes of depression and anxiety do not have to be due to a military activity. Rather, the cause merely needs to have happened during service. Oftentimes veterans are experiencing problems not directly related to the military that still affect their functioning during service. For example, if a veteran is deployed to another country and they are experiencing problems with their family at home, they might become depressed and anxious over their inability to be with their family while stationed abroad. Again, as long as the factors causing the veteran’s symptomatology, or the symptomatology itself, manifested during service, they are eligible for service connection.
Secondary Service Connection: “My service-connected disability caused my depression and anxiety.”
Service connection for depression and anxiety may also be established on a secondary basis. In this case, an already service-connected condition aggravates or causes the veteran’s depression and/or anxiety. For example, if the veteran is service-connected for a very debilitating back condition, it is possible that they will develop depression due to the chronic pain and limitations on activities of daily living. When filing for secondary service connection, providing a nexus opinion is especially important. The nexus between the veteran’s primary service-connected condition and their secondary condition must be clearly established in order to be granted secondary service connection for the latter.
Do I Have to File Separate VA Claims for Depression and Anxiety?
No. Importantly, VA recognizes that veterans are not qualified psychological experts. Veterans can only attest to their symptomatology and how it affects them on a daily basis. Therefore, it is unreasonable to expect veterans to be certain of their exact mental health diagnosis or whether two different conditions exist.
Clemons v. Shinseki (2009) held that a service connection claim for one psychiatric condition (e.g., PTSD) must be considered a claim for any psychiatric condition that may be reasonably raised by several factors (e.g., the veteran’s description of the claim and/or symptoms, evidence submitted by the veteran or obtained by VA). In other words, if there are other psychological diagnoses on record, VA is required to consider whether those diagnoses are related to a veteran’s service even if the veteran did not specifically file claims for those conditions. In short, veterans do not have to file separate VA claims for depression and anxiety.
How Does VA Diagnose or Evaluate My Depression and Anxiety for VA Disability Benefits?
From a diagnostic perspective, VA relies on the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition (DSM-5) published by the American Psychiatric Association (APA) to rate all mental health conditions. Again, for PTSD there is criterion requiring a stressor ; however, depressive and anxiety disorders have separate diagnostic criteria. As long as the veteran’s particular symptoms meet the frequency, duration, and severity outlined for those conditions in the DSM-5, they should receive proper diagnoses. Once a diagnosis is reached, VA will apply the General Rating Formula for Mental Health Conditions found under 38 CFR § 4.130.
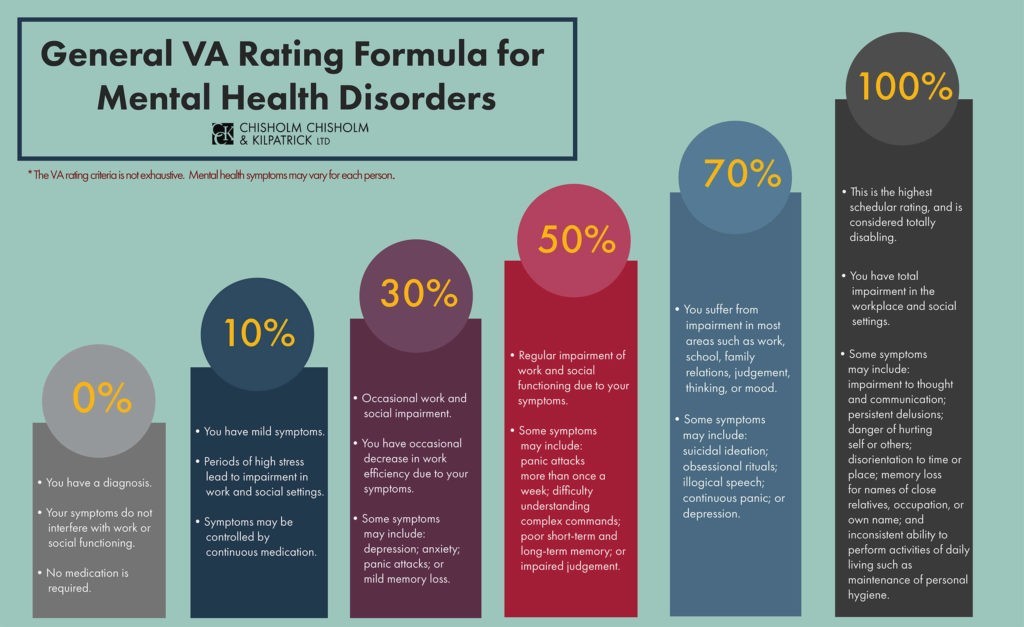
The possible disability ratings are: 0, 10, 30, 50, 70, and 100 percent. All mental health disability ratings are based on the severity of the condition and the resulting level of social and occupational impairment.
0% VA Rating for Depression and Anxiety
The 0 percent rating is reserved for a very mild presentation of psychopathology. If VA awards a 0 percent rating for depression or anxiety, it has determined that the veteran has a qualifying diagnosis, but the symptoms do not result in functional impairment or require medication. Importantly, a 0 percent disability rating is non-compensable, meaning the veteran will not receive monthly payments for that condition.
10% VA Rating for Depression and Anxiety
A 10 percent disability rating also represents a less severe form of depression or anxiety. The veteran may experience mild periods of high stress resulting in minor social and occupational impairment. However, the condition does not cause any major functional impairment and can be managed with medication.
30% VA Rating for Depression and Anxiety
The 30 percent rating criterion for depression and anxiety are also meant to represent mild symptomatology. In this case, “occasional decrease in work efficiency and intermittent periods of inability to perform occupational tasks” might mean that the veteran is starting to periodically miss work due to their lack of motivation associated with their mental health condition. However, their depression and/or anxiety does not fully prevent them from performing and succeeding in a work environment. Furthermore, they may occasionally isolate themselves as a result of their depressed mood and anxiety. Nonetheless, they are still able to maintain relationships with others. Overall, a 30 percent VA disability rating for depression and anxiety is assigned when a veteran presents with these symptoms in a mild manner, intermittently over time.
50% VA Rating for Depression and Anxiety
The 50 percent rating criterion involves an escalation in the frequency, duration, and severity of symptomatology. Furthermore, there are several additional symptoms included in this criterion that were not included in lower ratings. If veterans receive a 50 percent rating for depression and/or anxiety, it is likely that they are beginning to display more noticeable cognitive deficits such as difficulty following instructions or making decisions that depart from past behavior. Additionally, some of the mood-associated symptomatology may begin to manifest in physiological ways, such as a flattened affect. In other words, due to feelings of depression, veterans might speak in a monotonous tone and lack facial expressions. Overall, the level of occupational and social impairment also increases as part of the 50 percent rating. Here, the symptoms mentioned above cause a decrease in veterans’ ability to efficiently complete work-related tasks.
70% VA Rating for Depression and Anxiety
The 70 percent disability rating criterion for depression and anxiety is the most inclusive insofar as it represents a wide array of symptoms, including a progression of symptoms noted in the lower disability ratings. A veteran who receives a 70 percent rating for depression and/or anxiety may suffer from all of the symptoms included in the 50 percent rating, but at a higher frequency, duration, and severity. Here, the veteran is almost always in a state of panic or depression that affects their ability to interact with others. The veteran may also have trouble controlling their emotions in a way that leads to violent outbursts or conflicts with others. The level of social and occupational impairment may be evidenced by the veteran’s inability to hold down a job or complete classes for school.
100% VA Rating for Depression and Anxiety
The 100 percent rating is often difficult to obtain through VA because it requires a veteran’s symptoms to be so severe that they are totally impaired and unable to function in everyday life. While the symptoms listed in the 70 percent rating criterion involve a high level of impairment, the jump to 100 percent remains significant. There is often a substantial decline in cognitive and emotional functioning as compared to the rating criteria for lower percentages. Importantly, this decline results in total impairment when it comes to a veteran’s work life and personal life. An intermittent inability to perform activities of daily living can involve a veteran feeling too depressed to get out of bed, take a shower, or change clothes.
Self-injurious behaviors and suicide attempts are consistent with a 100 percent rating. In addition to thoughts and tendencies toward self-harm, a 100 percent rating for depression and/or anxiety also includes homicidal ideation in which a veteran may have thoughts of harming others. All of these symptoms and behaviors are consistent with the highest level of impairment reflected by the 100 percent rating criterion.
When Can I Get Separate VA Ratings for Mental Health Conditions?
VA’s General Rating Formula for Mental Health Conditions is meant to apply to a variety of psychiatric diagnoses. Veterans are not going to receive separate disability ratings for each mental health condition. Instead, they are going to receive a single disability rating under this formula that considers and accommodates all of their particular symptoms. For example, both depressed mood and anxiety are listed as symptoms in the rating criteria. Therefore, it is not a matter of getting separate ratings for each condition, but rather a matter of figuring out the severity of those symptoms and determining what the rating should be based on the level of social and occupational impairment that is present.
However, this is not to say that certain mental health conditions cannot be rated separately if deemed appropriate; for example, VA does have a separate set of criteria for eating disorders outside of the General Rating Formula. As such, there are certain circumstances where separate ratings may be involved, but they are few and far between. For the most part, mental health conditions are going to be rated together.
Can I Get Total Disability if My Depression and Anxiety Leave Me Unable to Work? (TDIU)
In some cases, a veteran’s depression and anxiety are so severe that they are unable to secure and maintain substantially gainful employment. Here, veterans can apply for total disability based on individual unemployability (TDIU) benefits. Importantly, TDIU provides monthly compensation at the 100 percent level even if a veteran’s combined disability rating is less than 100 percent. In theory, a veteran may be underrated for depression and anxiety at 50 or 70 percent. However, if they can show that they are unable to work as a result of their depression and anxiety, they may be entitled to TDIU.
What Evidence Should I Use to Show Both Depression and Anxiety?
VA often overlooks a diagnosis unless it appears clearly in the record. A veteran should submit:
- Mental health treatment records (VA or private) that list major depressive disorder, persistent depressive disorder, generalized anxiety disorder, panic disorder, or any other relevant diagnosis.
- Psychiatric evaluations or psychological testing that formally diagnose each condition.
- Medication records demonstrating treatment for both depressive symptoms (for example, SSRIs) and anxiety symptoms (for example, benzodiazepines, beta blockers).
This ensures that the conditions are “reasonably raised by the record,” which VA must consider under Clemons v. Shinseki, 23 Vet.App. 1 (2009).
Lay Evidence Differentiating Symptoms of Depression and Anxiety
Even if VA ultimately combines the conditions, describing your distinct symptom clusters helps VA account for the full severity of your condition.
For Depression:
- Loss of motivation, anhedonia, or inability to engage in hobbies
- Persistent sadness or hopelessness
- Sleep changes not tied to anxiety (for example, oversleeping)
- Low energy or fatigue
- Impaired concentration or slowed thought processes
- Suicidal ideation, even without plan or intent
For Anxiety:
- Excessive worry, restlessness, or hypervigilance
- Panic attacks (frequency is directly tied to rating levels)
- Physical anxiety symptoms (racing heart, sweating, shaking)
- Avoidance behavior or fear-based impairment
- Irritability or tension triggered by stressors
- Difficulty adapting to stressful circumstances
You should accurately and honestly describe frequency, duration, severity, and functional impact, because these factors directly map onto the General Rating Formula.
Lay Statements from Family, Friends, or Co-Workers
Third-party statements give VA independent confirmation of the distinct ways each condition affects functioning.
Helpful examples include:
- A spouse noticing withdrawal or lack of motivation (depression).
- A coworker observing panic episodes or inability to handle stress (anxiety).
- A family member witnessing irritability, sleep disturbance, or decline in grooming.
Statements should emphasize how symptoms impact employment, relationships, and daily living, because these are rating criteria.
Evidence About the Combined Impact of Depression and Anxiety
Even though the conditions share symptoms, it is critical to show VA the additive effect of having both.
Examples:
- Work records showing decreased productivity, disciplinary issues, or absences.
- School or training records showing difficulty concentrating or completing tasks.
- Documentation of panic episodes interfering with tasks or decision making.
- Reports of prolonged depressive episodes affecting reliability, motivation, or communication.
This evidence supports higher evaluations because § 4.130 focuses on occupational and social impairment, not on the diagnostic label.
Denied or Underrated for Depression and Anxiety? Contact CCK Law
Mental health claims can be exhausting, traumatizing, and inconsistently rated. If you disagree with a VA decision related to your claim for depression and anxiety, consider asking a VA-accredited attorney or advocate for help.
CCK Law has represented more than 36,000 veterans or dependents before VA or the U.S. Court of Appeals for Veterans Claims, and we may be able to help you as well. Our extensive experience means that we have seen how VA makes decisions and what arguments are the most efficient. Contact us online or at (800) 544-9144 to discuss your case.

Are You a Veteran in Crisis or Know of One?
Please be advised, VA has implemented the Veteran Crisis Line equipped with specially trained responders ready to help veterans 24 hours a day, 7 days a week, 365 days a year. The Veterans Crisis Line connects service members and veterans in crisis, as well as their family members and friends, with qualified, caring VA responders through a confidential toll-free hotline, online chat, or text messaging service. Veterans can access the Crisis Line in any of the following ways:
- Dial 988 and Press 1 to talk to someone
- Send a text message to 838255 to connect with a VA responder
- Start a confidential online chat session at VeteransCrisisLine.net/Chat
- Take a self-check quiz at VeteransCrisisLine.net/Quiz to learn whether stress and depression might be affecting you
- Find a VA facility near you
- Visit MilitaryCrisisLine.net if you are an active duty service member, guardsman, or reservist
If you or someone you know is currently experiencing a crisis, please seek assistance through the resources listed above.
About the Author
Share this Post
