Can Your Benefits Be Terminated While on Long-Term Disability?
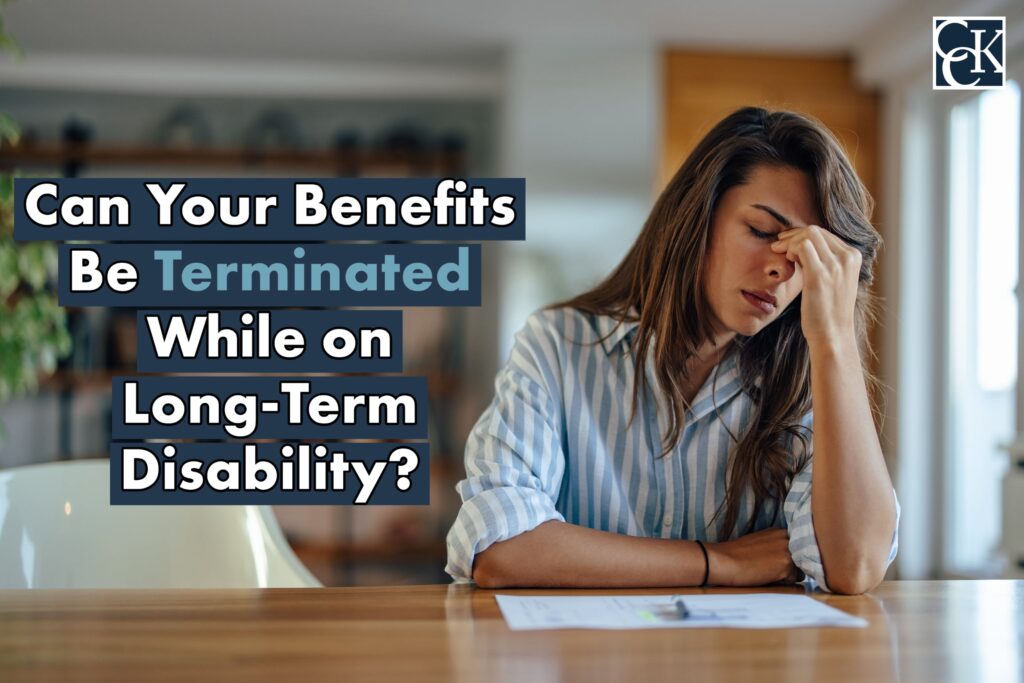
Long-term disability (LTD) claims can be challenging and time-consuming. Long-term disability insurance coverage can help protect a percentage of your income when you are unable to return to work due to a debilitating medical condition or injury. Many, though not all, LTD policies allow benefits until retirement age. Unfortunately, even once your long-term disability claim is approved, your benefits can still be terminated.
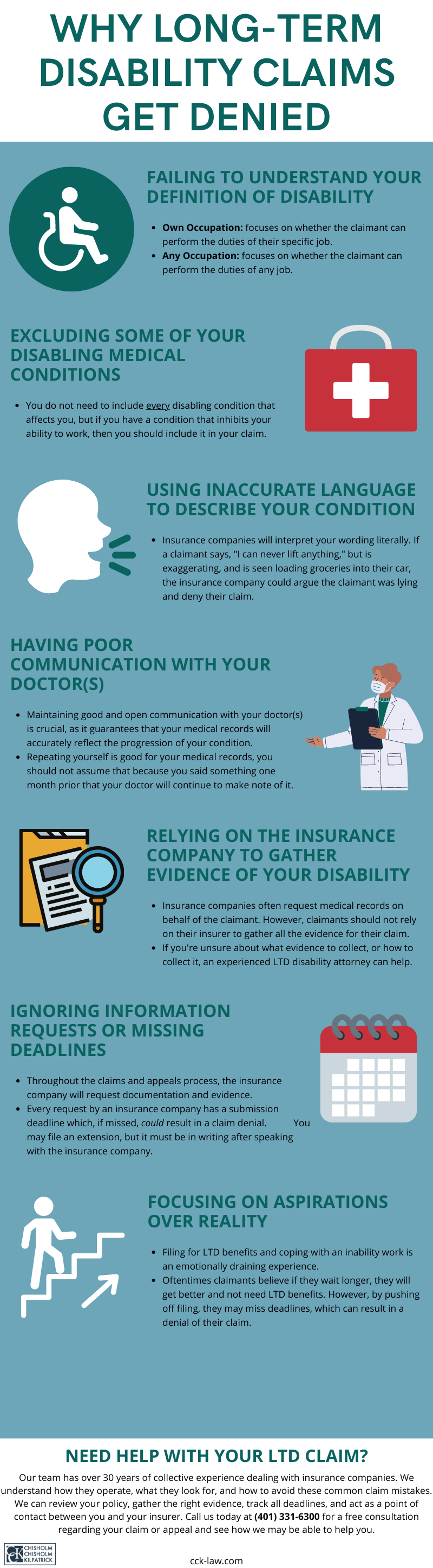
There are many reasons why the insurance company may terminate your benefits. Your claim may be terminated if you are no longer disabled since you no longer meet the definition of disability. In many policies, the definition of disability changes after 24—48 months and will then consider whether you are disabled from any occupation, not just your own occupation.
There can also be other limitations in your policy that could result in termination. Below, we discuss some of the reasons why your long-term disability claim may be terminated, but you should read your policy carefully to understand the definition of disability and other factors and provisions that may affect your ability to continue receiving long-term disability benefits.
Medical Reviews
From time to time, the insurance company may conduct medical reviews of your claim to determine if you continue to meet the applicable definition of disability. They will often review the medical records they have on file and request updated medical records from your providers. They may also check to see whether you continue to receive medical treatment for your condition.

The insurance company may even hire a third-party nurse or doctor to review the medical records. You should keep in mind that many of these nurses or doctors are repeatedly hired by insurance companies to conduct reviews. Your benefits could be terminated if the third-party reviewer determines that you do not have restrictions or limitations that prevent you from working. You should contact an attorney if your insurance company is conducting a medical review and you do not think the medical evidence is being assessed fairly.
Vocational Reviews
If your policy changes to an any occupation definition of disability after a certain period of time, your insurance company may have a vocational specialist review your claim to determine if you are capable of working in another occupation. If the vocational specialist determines that you are capable of performing other occupations, your long-term disability claim may be terminated. The specialist may suggest different occupations that you feel are not consistent with your medical condition or vocational skills. It can be challenging to counter these vocational reviews. You should contact an attorney if you disagree with the occupations suggested by the vocational specialist.
Application of Policy Limitations and Terminated Benefits
It is very important to read your policy entirely to locate and understand any limitations that may be involved with your claim. Many policies have limitations that restrict the amount of time that benefits are payable depending on your disabling condition(s). For example, many policies will limit disabilities based on mental health conditions to 12 to 24 months of benefits.
If your disability is primarily due to a mental health condition and your policy contains such a limitation, the insurance company may terminate your claim once you receive the maximum number of benefits, even if you continue to meet the applicable definition of disability.
Not Cooperating with the Insurance Company and Terminated Benefits
Many policies will have a provision requiring you to comply with the insurance company’s information requests in order to remain eligible for benefits. While you are receiving benefits, the insurance company will periodically send claim update forms and requests for updated medical records. It is important that you continue to fill out the forms and remain consistent with the previous forms you completed. Although this can appear repetitive, the termination of disability benefits may happen if you fail to comply or do not provide the information requested by the insurance company.
Contact Chisholm Chisholm & Kilpatrick
At Chisholm Chisholm & Kilpatrick LTD, our team of attorneys and professionals has the experience to advocate for the benefits to which you are rightfully entitled. We understand that having your long-term disability benefits terminated can be scary and frustrating. You want to receive benefits that will help you manage your condition. We can help you get back on claim and stay there. Our team is familiar with ERISA law, which often governs LTD policies, and we will work to ensure that your claim receives a fair review. Call CCK today at (800) 544-9144 for a free case evaluation consultation. A member of our team will analyze your case and determine if we can assist you.
About the Author
Share this Post