Mood Disorders and VA Disability Benefits
CCK Law: Our Vital Role in Veterans Law
What Are Mood Disorders?
Mood disorders, oftentimes referred to as affective disorder, are a mental health conditions that severely impacts mood and its related functions. Importantly, “mood disorders” is an umbrella term used to represent different types of mental health conditions, including the following:
- Major depressive disorder – prolonged and persistent periods of extreme sadness
- Bipolar disorder (types I and II) – involves alternating periods of depression and mania
- Persistent depressive disorder – a long-term (chronic) form of depression
- Cyclothymia – a disorder that causes emotional ups and downs that are less extreme than bipolar disorder
- Seasonal affective disorder – a form of depression most often associated with fewer hours of daylight in the far northern and southern latitudes of late fall to early spring
- Premenstrual dysphoric disorder – mood changes and irritability that occur during the premenstrual phase of a woman’s cycle and dissipate with the onset of menses
- Depression related to medical illness – persistent depressed mood and a significant loss of pleasure in most or all activities that is directly related to the physical effects of another medical condition
- Depression induced by substance use or medication – depression symptoms that develop during or soon after substance use or withdrawal or after exposure to a medication
With the update of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) in 2013, mood disorders are now separated into two groups: (1) bipolar disorder and related disorders and (2) depressive disorders. Nonetheless, the above-mentioned mood disorders fall somewhere within those two categories.
Mood disorders can often lead to significant social and occupational impairment. Generally speaking, symptoms of mood disorders may include the following:
- Anhedonia (i.e., loss of pleasure)
- Changes in appetite (i.e., eating more or less than usual)
- Sleep impairment (i.e., difficulty falling/staying asleep, early morning awakening)
- Fatigue
- Crying spells/tearfulness
- Anxiety
- Flat affect
- Feelings of hopelessness/worthlessness
- Social isolation/withdrawal
- Difficulty concentrating and decision-making
- Feelings of guilt
- Irritability
- Suicidal thoughts
Although there is no exact cause of mood disorders, research indicates that a variety of factors contribute to these conditions. For example, chemical imbalances in the brain, as well as stressful life events (e.g., death, divorce, trauma), may both lead to the development of a mood disorder.

How are Mood Disorders Diagnosed?
Mood disorders should be diagnosed by a mental health professional, such as a psychologist or psychiatrist. They may ask a series of questions related to an individual’s mood, recent life stressors, active symptoms, and level of impairment. From there, the mental health professional will use the DSM-5 to make an appropriate diagnosis. Oftentimes, a primary care provider will perform a physical examination and lab tests to rule out any physical reasons for mood-related symptoms in conjunction with the psychological evaluation.
Treatment for Mood Disorders
The majority of individuals with mood disorders are able to return to a baseline level of functioning with proper treatment and intervention. Treatments for mood disorders typically include a combination of psychotherapy (i.e., talk therapy), such as cognitive-behavioral therapy or dialectical behavior therapy, and medications.
VA Service Connection for Mood Disorders
Direct Service Connection
To establish direct service connection for mood disorders, veterans must demonstrate the following: (1) a current diagnosis of a mood disorder; (2) an in-service event, injury, or illness; and (3) a medical nexus linking the current, diagnosed mood disorder to the in-service occurrence. Most often, veterans must provide evidence of treatment records either during or following service to show the presence and severity of their mood disorder. From there, VA will typically schedule the veteran to attend a Compensation & Pension (C&P) examination to obtain a medical nexus.
Secondary Service Connection
Secondary service connection is established when a veteran demonstrates that an already service-connected condition causes a subsequent condition to develop. In this case, a veteran’s mood disorder may qualify as a secondary condition. For example, a veteran has a severe back condition that limits them from engaging in their daily activities. Due to the loss of autonomy, immobilization, and inability to engage in things they enjoy, the veteran begins experiencing symptoms of depression. Several months later, the veteran is diagnosed with major depressive disorder. The veteran’s major depressive disorder may qualify for service connection on a secondary basis seeing as it developed as a result of their already service-connected back condition.
How VA Rates Mood Disorders
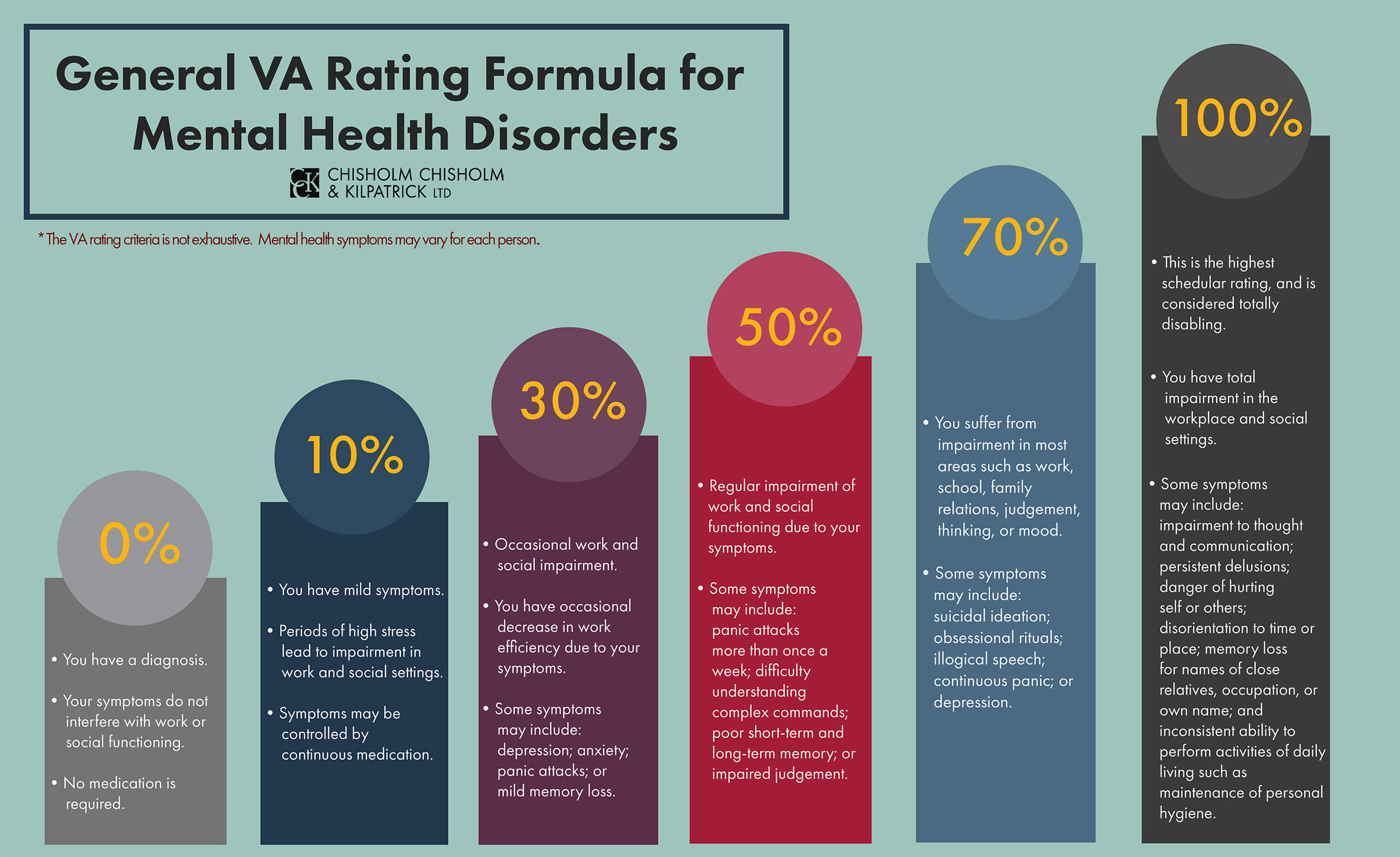
Aside from eating disorders, VA rates all eligible mental health conditions using the same diagnostic criteria outlined under 38 CFR § 4.130. Specifically, mental health conditions are rated at 0, 10, 30, 50, 70, or 100 percent using VA’s General Rating Formula for Mental Disorders. These ratings are based on the level of social and occupational impairment caused by the condition. For example, a veteran experiencing mild symptoms, or whose symptoms are well controlled by continuous medication, may receive a disability rating of 10 percent. Veterans with more severe symptoms, such as an intermittent inability to perform activities of daily living, may receive a 100 percent disability rating.
Importantly, veterans are not required to meet all, or even any, of the criteria in a rating level to qualify for that rating. Since mental health conditions can manifest differently per individual, VA’s rating formula for mental health conditions is not binding. Instead, symptoms listed in each level of the rating formula are simply examples to demonstrate the types and levels of impairment commonly found at that assigned percentile rating.
About the Author
Share this Post