Getting Long-Term Disability (LTD) Benefits for Melanoma

Melanoma is a serious form of skin cancer that develops in the cells, known as melanocytes, that produce melanin, the pigment that gives your skin its color. While melanoma may not be disabling on its own, the therapies that are used for treatment often come with debilitating side effects that may leave you unable to work.
This article will explore melanoma and how it can disable a person from working. It will also discuss how to get long-term disability (LTD) benefits for melanoma, and more.
Can Melanoma Qualify for Long-Term Disability Benefits?
Long-term disability benefits are contingent upon whether a claimant can prove that their condition prevents them from working under the terms of their policy. Every LTD insurance policy contains a definition of disability that claimants must meet to receive benefits.

While melanoma may not be disabling on its own, the therapies that are used for treatment often come with debilitating side effects that may leave you unable to work. For example, most of these treatments cause chronic fatigue, which would leave you with less energy during the day and may require you to take frequent breaks or naps, rendering you unable to perform your work efficiently.
Another common side effect, specifically from chemotherapy, is peripheral neuropathy in the upper or lower extremities. This side effect causes numbness, weakness, and pain in the affected areas and can impact your ability to stand or walk, as well as interfere with fine manipulation tasks like typing and writing, depending on which area of the body is affected.
Additionally, immunotherapy and targeted therapies can cause headaches, muscle aches, and general malaise that can lead to reduced stamina, pain that is distracting, and certain physical limitations like being unable to sit for most of the day. Lastly, many of these treatment options are accompanied by cognitive difficulties, commonly referred to as “chemo brain,” that may impact your ability to concentrate, multitask, remember, and pay attention to detail.
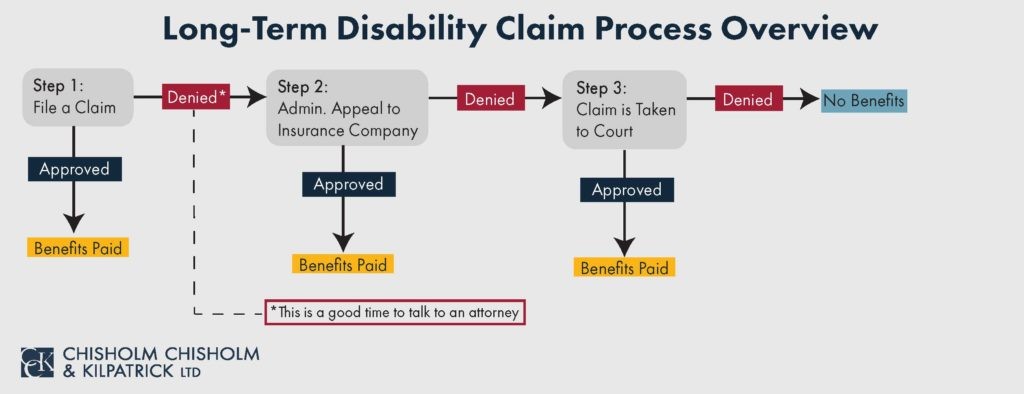
If LTD claimants can show, through evidence, that their melanoma treatment is disabling them under the terms of their policy, then they should qualify for such benefits. However, insurance companies frequently deny LTD claims. In such scenarios, it is often best to contact an experienced ERISA attorney to help.
What Happens If a Melanoma LTD Claim Is Denied?
If an insurance company denies a long-term disability claim, then it will send the claimant a denial letter. Claimants who receive a denial of their claim have the right to file an administrative appeal.
A long-term disability lawyer can help individuals with melanoma receive LTD benefits. Some of the ways an experienced LTD attorney can help include:
- Reviewing the denial letter
- Gather and analyze the claimant’s claim file
- Gather medical records from treatment providers
- Gather additional evidence, such as vocational evaluations, to supplement the claim
- Litigate when necessary
The long-term disability claims and appeals process can be an arduous process, but it is not one a person with melanoma must face alone.
Call Today to Speak with a Member of Our Team
CCK can help you fight the insurance company and level the playing field by using our knowledge and experience with ERISA, the U.S. Department of Labor Regulations, and various insurance policies. We take a comprehensive approach to long-term disability appeals, gathering supportive evidence that objectively demonstrates your disability and writing a strong appeal based on that evidence.
Let us help you. Call Chisholm Chisholm & Kilpatrick today at (800) 544-9144 for a free case evaluation to see if we can fight for you.
Share this Post