Navigating Your Long-Term Disability (LTD) Insurance Claim Through the COVID-19 Pandemic
This is an unprecedented time in our lives and many people are facing uncertainty, whether it be professionally, financially, or medically. We have needed to adjust rapidly to changing circumstances, frequently and with little warning. While the current situation is challenging for everyone, it can be especially difficult if you are medically unable to work. In this blog, we address some questions that you may have about handling your long-term disability (LTD) insurance claim in the midst of the coronavirus pandemic.
What If I Have a Health Condition That Places Me at High Risk If I Were to Contract COVID-19?
Due to COVID-19, many businesses have shut down altogether or have transitioned to remote work. However, there are some essential businesses that must remain open and cannot be done remotely. If your job still requires you to go to work each day and you have a health condition that makes exposure to COVID-19 a high risk for you, you may be eligible to file a disability claim.
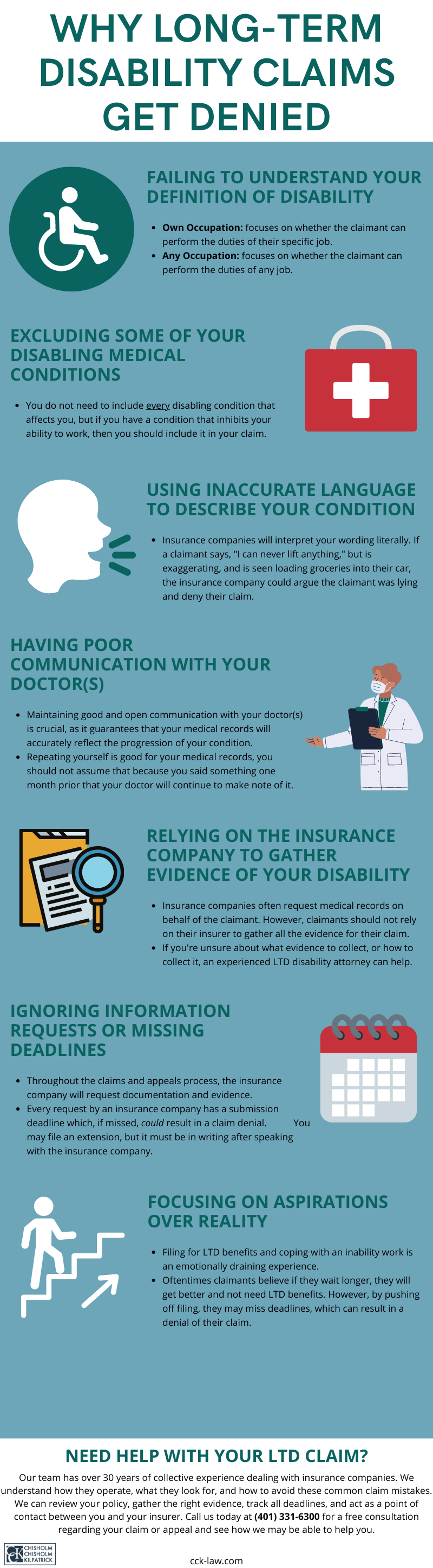
The first step you should take is to read your disability insurance policy, as that determines the coverage that is available to you. Among other things, your policy will tell you what definition of disability you need to meet and whether there are any exclusions from your coverage. Whether you can receive disability benefits due to your high health risk depends on the terms of your policy. For example, some policies exclude risk to health as a basis for disability, if you are otherwise capable of performing your occupation.
Additionally, some disability policies exclude coverage for pre-existing conditions. While the specific terms of this exclusion will vary from policy to policy, if you only recently obtained your coverage and were treated for your health condition prior to obtaining it, then your disability may be excluded from benefits.
Even if it appears that your policy allows for such a claim, you must also submit evidence of your disability. You will need a doctor to certify that your health condition places you at risk if you were to be exposed to COVID-19. Although there is no definitive level of risk required, typically, the risk must be sufficiently high for it to be considered disabling. In addition, you will likely need medical records documenting that you have been diagnosed with, and treated for, the health condition that places you at high risk.
Unfortunately, even if your disability policy does not explicitly preclude such claims and you can provide all of the above evidence, these claims are still likely to be difficult and one should expect the insurance company to fight them.
What If I Need to File a Disability Claim for Reasons Unrelated to COVID-19?
Rather than being unable to continue working due to COVID-19, you may become unable to work for unrelated reasons, but the pandemic is still likely to have a significant impact on your disability claim.
Reading your disability insurance policy is still an important first step in understanding what definition of disability you need to meet and what kind of evidence you need to submit in support of your claim. Usually, you will be required to submit a claimant’s statement, an attending physician statement, and medical records.
The claimant’s statement is your opportunity to explain, in your own words, what prevents you from working. You should not limit yourself to the small space the insurance company provides – if an explanation of your condition, symptoms, or treatment requires additional space, submit an attachment with the original form.
For attending physician statements, we typically recommend that claimants make appointments with their treatment providers in order for them to complete this form. This helps ensure that your doctor documents all of the conditions and symptoms that impact your ability to work, and that they do so accurately.
However, in light of COVID-19, many doctors’ offices are postponing or canceling non-emergency appointments. Some are providing telephone or video appointments instead. If an in-person appointment is not possible, telemedicine is likely the next best option. This will allow you to still communicate with your doctor while they are completing the form and ensure that they are responding to the insurance company’s questions completely and accurately.
The insurance company will often request medical records on a claimant’s behalf, but it ultimately remains the claimant’s responsibility to provide the records and proof of disability. With many doctors’ offices closed, obtaining your medical records may be challenging.
If you are having difficulty obtaining your records, there are additional kinds of evidence you can submit to demonstrate your disability. For example, you can create a symptom log, which documents when you experienced symptoms of your disabling condition, what those symptoms were, how long the symptoms lasted, how those symptoms impacted you, and what you needed to do to treat them.
Additionally, you can ask friends, family members, or co-workers to write statements regarding their observations about how your disabling condition impacts you both professionally and personally. Finally, if your disability or its resulting symptoms are outwardly visible, you can use photos or videos to document them.
How Will COVID-19 Impact Me If I Am Already Receiving LTD Benefits From an Insurance Company?
COVID-19 may also affect your LTD claim if you are already receiving benefits. Even when your claim is approved, you must periodically provide updated information to the insurance company that demonstrates that you are continuing to meet the applicable definition of disability. Like an initial claim, these updates can include claimant forms, attending physician statements, and updated medical records. The recommendations above for filing an initial claim are equally applicable to updates for an already existing claim.
Some insurance companies may be simply continuing already approved claims and not conducting updates during this time. However, that is not the case for all companies, and you should complete an update to the best of your ability if one is requested. Ignoring the insurer’s update request or failing to respond by the deadline is likely to lead to a claim termination. If you are having difficulty responding to the insurance company’s requests, say that to your insurer and document your communications. While you cannot guarantee that this will prevent your insurer from terminating your benefits, you will at least have some evidence of the unreasonableness of their decision.
What If My LTD Claim Was Denied and I Need to File an Appeal During COVID-19?
If your LTD claim was denied or your benefits were terminated, you have the right to appeal the insurance company’s decision. However, there is typically a limited amount of time to do so.
You should first review the insurance company’s denial letter to determine what information or evidence it claimed was missing or on which medical opinions it based its denial. You can also request a copy of your claim file from the insurance company, which should include the insurer’s notes, as well as any medical records or opinions on which it relied in making its determination.
You should then gather your medical records, as well as reports from your treating physicians, explaining why you are disabled and responding to the insurance company’s basis for denying benefits. Once you have gathered all the necessary evidence, it should be submitted to the insurance company with a letter documenting that you are appealing and explaining why the insurance company’s decision to deny benefits was wrong.
If you are having difficulty obtaining medical records or reports from your doctors, you can submit alternative forms of evidence, such as those discussed above. However, the administrative appeal is often your last opportunity to get evidence into the record prior to litigation under ERISA, so you need to make sure that all evidence is submitted to the insurance company prior to the appeal deadline. If necessary, you can request an extension of time from the insurance company. If one is granted, you should ensure that this extension is in writing.
Given the importance of the administrative appeal with the insurance company, it is a good time to consider getting an attorney involved.
Contact Us For a Free Case Evaluation
Chisholm Chisholm & Kilpatrick is fully operational and handling cases for clients during the COVID-19 pandemic. We are experienced ERISA and insurance litigators who can help you obtain the benefits to which you are entitled. If your disability claim is denied or your benefits are terminated, you have the right to appeal that decision. Regardless of your specific situation, you do not need to face it alone. Contact us at 401-331-6300. Our case evaluation to find out if we can assist is free, and we often represent clients on a contingency basis, which means that we are only paid if we win your claim; and you do not pay upfront fees out of pocket.
About the Author
Share this Post