How to Apply for Long-Term Disability (LTD) Benefits

Many employers offer long-term disability (LTD) coverage as a benefit to their employees. If you become unable to work due to a medical condition and you are covered under an employer-provided long-term disability plan, you should contact your human resources department to obtain a copy of your long-term disability plan’s governing documents so you can determine the process to apply and file a claim. Often, applying for social security disability benefits is required as part of the LTD claim process.
Your policy contains a lot of information, such as the waiting period, which can often be covered by short-term disability coverage; how to appeal; filing deadlines; and more. Nonetheless, you are ultimately responsible for ensuring that evidence of your disability is submitted to the insurance company when you apply for LTD benefits.
Long-Term Disability Claim Forms
When a person stops working, they must consider LTD benefits. One of the first things in the application process to be done is complete claim forms. Insurance companies require such forms when filing a claim. When you apply for long-term disability benefits, be sure to list specific reasons why you cannot do your job due to your disability. You should not simply say that you cannot work because of your condition.
You should make sure to note how the condition affects your ability to work and your day-to-day life. You should not feel limited to the space provided to write your information and can attach additional pages to the claim forms if desired. Consider contacting a disability attorney if you are unsure what you should do to strengthen your claim.
Your employer will be required to fill out some paperwork regarding your disability claim as well. Typically, your employer will need to answer questions regarding your job duties, your salary, and when you stopped working.
Insurance companies often require you to have your doctor(s) complete forms for your claim. These forms are typically called “Attending Physician Statements” (APS). It is important that you discuss the APS directly with your provider before giving them the form in order to make sure they are supportive of your claim and will advocate for you on the APS. If they are not supportive and they complete the form, it could hurt your claim and result in a denial of benefits.
Like the forms you will need to complete yourself, your doctor should not simply write that you cannot work. Instead, they should include what about your condition specifically prevents you from working.
Medical Records
In addition to the claim forms, you should gather the medical records from your treating providers to submit to the insurance company. You may also need to obtain reports or statements from your doctors if your medical records do not fully or accurately document your disabling condition.
You should not rely on the insurance company to request all the medical records pertinent to your disability, but instead should gather the medical records yourself and make sure that you have all the documentation required to make your claim as strong as possible.
You can also submit written statements from your family, friends, and coworkers to help provide further evidence of your disability. Because it is ultimately your responsibility to ensure that everything is submitted for your claim, it is wise to both request your medical records yourself and ensure that your providers respond to requests from the insurance company. Lack of compliance with the insurance company’s requests could lead to a claim denial.
Consistency
It is important to make sure that all of your evidence is consistent with the information you provided on the claim forms. This includes medical records, statements, and anything else you might submit. Once your claim is submitted, the insurance company may ask you for additional information or documentation. It is crucial to remain consistent with what you reported previously unless a true change in your condition has occurred.
When Will a Decision Be Made After I Apply for Long-Term Disability?
Generally, after you submit a long-term disability claim, the insurance company has 45 days to issue a decision. If they determine that additional time is required, they may provide notice in writing that they are taking an additional 30-day extension. The insurance company can take up to two 30-day extensions.
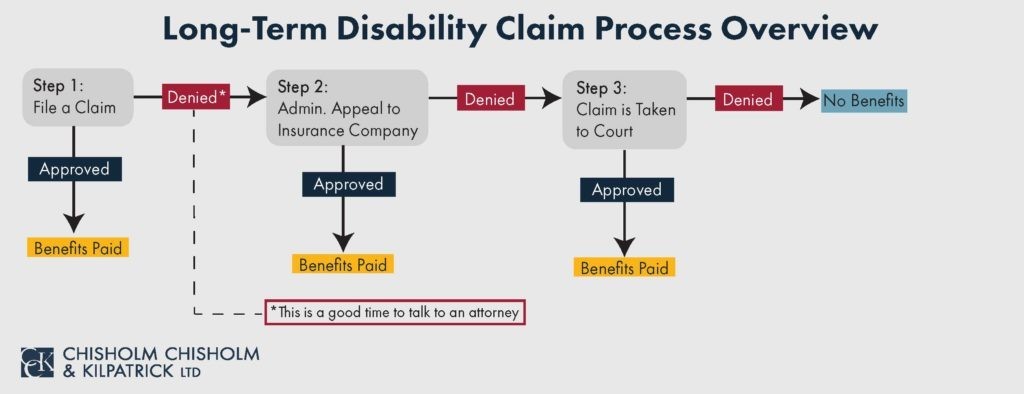
My Long-Term Disability Claim Was Denied – Now What?
You can appeal the insurance company’s denial of your long-term disability claim. Long-term disability appeals can be difficult and confusing. You typically have 180 days from the date noted on your denial letter to file an appeal. It is important that you do not take the appeal lightly. The appeal is typically a critical stage in the long-term disability claim process because it can be your last opportunity to get evidence onto the record under ERISA law.
You should consider contacting an attorney if your claim has been denied. They can help you build a strong appeal, including obtaining types of evidence that you may be unaware of such as vocational reports, functional capacity evaluations, and neuropsychological exams.
Contact CCK
At Chisholm Chisholm & Kilpatrick, our team of experienced attorneys and professionals know how challenging and time-consuming it can be to apply for long-term disability insurance benefits. You should not have to worry about your LTD insurance coverage. We have helped many clients receive the long-term disability benefits they deserve. Contact us now at (401) 237-6412 for a free case evaluation to see if we can assist you.
About the Author
Share this Post