VA Health Care Eligibility, Priority Groups, & Copays
CCK Law: Our Vital Role in Veterans Law
What is VA Healthcare?
The Veterans Health Administration (VHA) is the largest integrated healthcare system in the United States. It provides care at over 1,200 facilities and helps over 9 million veterans across the country. Each VHA facility is staffed with Patient Advocates who can answer any questions veterans may have about the healthcare system.
VA healthcare may include services related to:
- Vision and hearing
- Dental care
- Health exams & education
- Inpatient services (e.g., surgery)
- Mental health services
- And more
Requirements for VA Healthcare
Generally speaking, to qualify for VA healthcare, veterans who served in the active military, naval, or air service, must have received an other-than-dishonorable discharge and be service-connected for a qualifying condition. Importantly, the veteran’s disability rating does not matter.
VA’s requirements are as follows:
- If you enlisted after September 7, 1980, or entered active duty after October 16, 1981, you must have served 24 continuous months or the full period for which you were called to active duty, unless any of the descriptions below are true for you.
This minimum duty requirement may not apply if any of these are true. You:
- Were discharged for a disability that was caused—or made worse—by your active-duty service, or
- Were discharged for a hardship or “early out,” or
- Served prior to September 7, 1980
If you are a current or former member of the Reserves or National Guard, you must have been called to active duty by a federal order and completed the full period for which you were called or ordered to active duty.
If you had or have active-duty status for training purposes only, you do not qualify for VA health care.
Enrollment in VA Healthcare
VA’s budget is decided by Congress each year. The more money VA gets, the more veterans can enroll in VA healthcare. And, of course, the opposite is true—less money means fewer enrollees. For this reason, VA assigns every veteran an Enrollment Priority Group to make sure that certain groups of veterans can enroll before others.
When you apply for enrollment, VA will determine if you are eligible for VA healthcare and, if so, assign you a Priority Group. Your Priority Group also determines whether you will be responsible for copayments for medications and different types of care at VA Medical Centers.
Each priority group has a different copay, so if a veteran is moved from one group to another, their copay could change.
Below, you will find the types of veterans that fit into each Priority Group. You can reference the graphic as a starting place for determining which Group you may fall into but be aware that this is just an overview. You may want to check out the specific language VA uses to describe each group.
If you meet the requirements for more than one Priority Group, VA will place you in the highest Priority Group for which you are eligible.
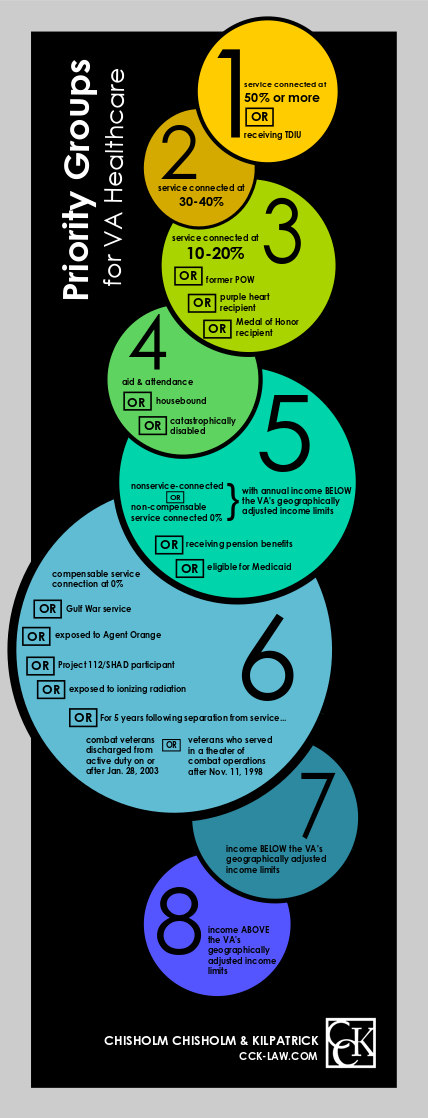
Priority Group One
Priority Group One is the highest priority group. In order to be placed in this group, the veteran will need to be service-connected at 50 percent or more, or be receiving total disability based on individual unemployability (TDIU). Additionally, veterans who received the Medal of Honor qualify for Priority Group One.
Priority Group Two
Veterans in Priority Group Two will need to be service-connected between 30 and 40 percent.
Priority Group Three
In order to be eligible for Priority Group Three, veterans will need to either be service-connected between 10 and 20 percent, be a former prisoner of war (POW), or be a Purple Heart recipient. You will also be eligible for this group if you were discharged for a disability that was caused or worsened by your active-duty service, or were awarded special eligibility classification under Title 38, U.S.C § 1151.
Priority Group Four
Veterans who qualify for Priority Group Four are those who receive benefits for housebound status or aid and attendance benefits. Additionally, veterans who VA has determined have a catastrophic disability are eligible.
Priority Group Five
Veterans who are receiving VA pension benefits or are eligible to apply for Medicare qualify for Priority Group Five. Veterans who are not service-connected or who are service-connected at the non-compensable level such as 0 percent are also eligible under this category.
Priority Group Six
In order to be eligible for Priority Group Six, veterans will need to meet one of the following:
- Have served in the Republic of Vietnam anytime between January 9, 1962 and May 7, 1975
- Are a veteran of the Persian Gulf War who served in active-duty military service between August 2, 1990 and November 11, 1998
- Are a veteran of World War I or the Mexican border period
- Have been awarded a 0 percent compensable rating for a disability related to active duty military service
- Were exposed to Agent Orange
- Currently or previously were a Project 112/SHAD participant
- Were exposed to ionizing radiation
- Completed at least thirty days of active duty military service at Camp LeJeune between August 1, 1953 and December 31, 1987
- Are a veteran or active duty military servicemember who served or is serving any time after November 11, 1998. Those whose active duty discharged occurred after January 28, 2003 will receive enhanced post discharge benefits for five years after being discharged.
Priority Group Seven
Those who qualify for Priority Group Seven will need to have a household income that is below VA’s income limit based on geographical location.
There are also two sub-groups within Priority Group Seven. They are Sub-priority A and Sub-priority B.
- Sub-priority A: Veterans who registered as of January 16, 2003 and who have remained continuously enrolled or had a change in eligibility status that required VA staff to place the veteran in this group are eligible under Sub-priority A.
- Sub-priority B: Veterans who were registered as of June 15, 2009 and whose annual income is 10 percent or less above VA’s geographically adjusted income limits are eligible under Sub-priority B.
Priority Group Eight
Priority Group Eight requirements are also based on VA’s geographically adjusted income limits, however, in order to qualify the veteran will need to have income above this threshold.
Similar to Priority Group Seven, there are two sub-priority categories within Priority Group Eight. They are Sub-priority group C and Sub-priority group D.
- Sub-priority C: Veterans who registered as of January 16, 2003 and who have remained continuously enrolled or had a change in eligibility status that required VA staff to place the veteran in this group are eligible under Sub-priority C.
- Sub-priority D: Veterans who were registered as of June 15, 2009 and whose annual income is 10 percent or less above VA’s geographically adjusted income limits are eligible under Sub-priority D.
Additionally, there are Sub-priority E and Sub-priority G, which do not provide for VA health care services. There is one exception, however, in that veterans who have been rated at a non-compensable 0 percent for their service-related disability may receive medical benefits that cover only their service-related injury or disability.
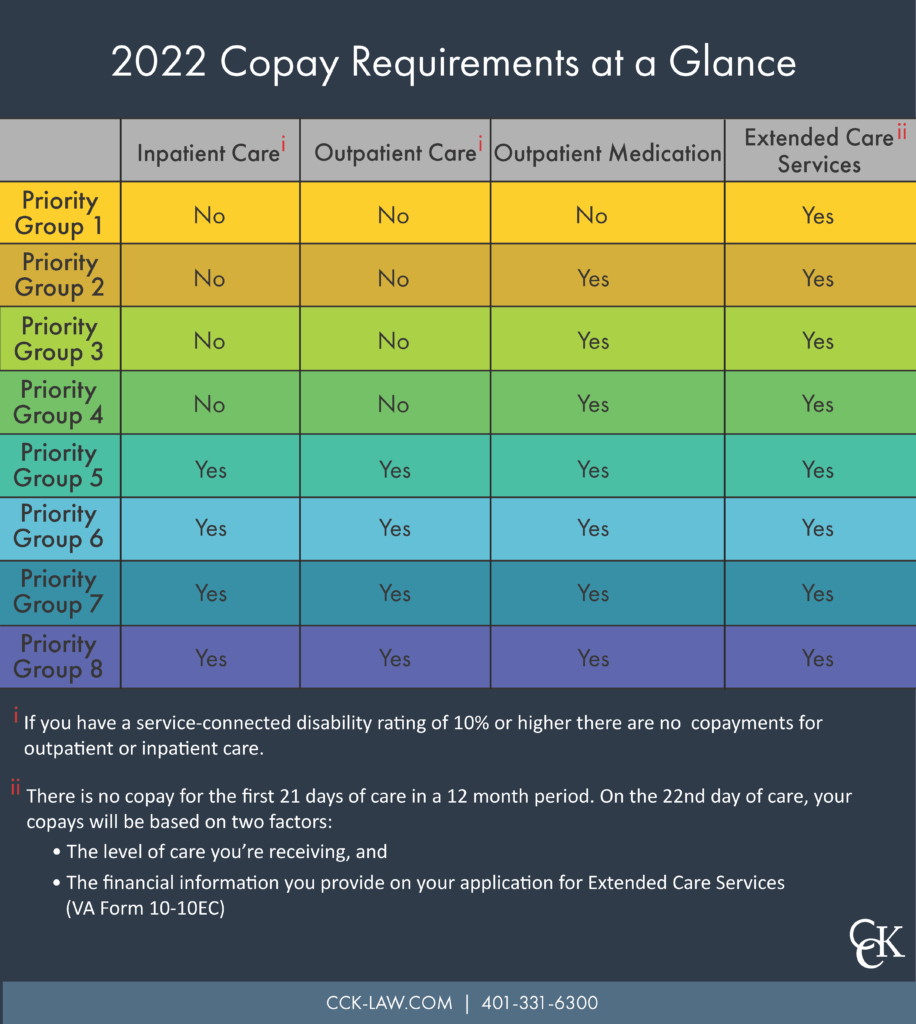
VA Healthcare Co-Payments for Each Priority Group
Under Medical Benefits Package, veterans in different priority groups typically have access to the same medical services (with some exceptions—see “Eyeglasses & Hearing Aids” below). But each Priority Group has different rules regarding a veteran’s responsibility for copayments.

VA Healthcare Services Exempt from Inpatient and Outpatient Copayments
The following services do NOT require inpatient and outpatient copays, regardless of the veteran’s Priority Group:
- Care related to a VA-rated service-connected disability
- Special registry examinations offered by VA to evaluate possible health risks associated with military service (for example, the Agent Orange Registry exam)
- Counseling and care for military sexual trauma
- Compensation and Pension examinations
- Care that is part of a VA research project
- Readjustment counseling
- Care for cancer of the head or neck caused by nose or throat radium treatments received while in the military
- Individual or group smoking cessation or weight reduction services
- Hospice care
OEF/OIF/OND Combat Veterans
As shown in the graphic above, combat veterans discharged from active duty on or after January 28, 2003 are eligible for enrollment in Priority Group 6 for 5 years following discharge, unless they qualify for a higher group. After the 5-year period ends, these veterans will be reassigned to the appropriate Priority Group and subject to copayment requirements, if applicable.
During the 5-year “enhanced eligibility” period, combat veterans in Priority Group 6 are, unlike other Group 6 members, responsible for copayments for care related to any conditions that are congenital or developmental (for example, scoliosis that existed before military service), or for specific ailments that began after service (for example, a common cold).
TIP: You can find this year’s copay amounts for different services on VA’s website.
Eyeglasses & Hearing Aids
VA healthcare covers routine vision and hearing exams and preventive tests, but generally does not cover eyeglasses or hearing aids.
However, VA will provide you with eyeglasses and/or hearing aids if you:
- Receive compensation for a service-connected disability (of any kind),
- Receive increased pension for regular aid and attendance or for being permanently housebound,
- Are a former Prisoner of War (POW), or
- Received a Purple Heart medal.
There are a few other scenarios in which veterans may obtain eyeglasses or hearing aids from VA. More information about VA’s eyeglasses and hearing aid policy is available on VA’s website.
Dental Care
VA only offers dental care benefits to certain qualifying veterans, based on a “Class” system. However, veterans who do not qualify for VA dental care (but are enrolled in VA healthcare) may purchase dental insurance at a reduced cost through the VA Dental Insurance Program (VADIP).
To find out more about VADIP or the system used to determine eligibility for VA dental benefits, you can visit this VA website.
How to Enroll in VA Healthcare
To enroll in VA’s Medical Benefits Package, you must apply (in most cases) by submitting VA Form 10-10 EZ by mail, in person, or online.
If you submit the form by mail, you should send it to:
Health Eligibility Center
Enrollment Eligibility Center
2957 Clairmont Road, Suite 200
Atlanta, GA 30329-1647
About the Author
Share this Post