Mental Health: How to Get VA Disability for Mental Health Conditions
CCK Law: Our Vital Role in Veterans Law
Veterans are more likely than non-veterans to struggle with mental health conditions. According to the American Psychiatric Association, one in 20 US adults has a diagnosable mental disorder; in comparison, research indicates that “approximately 14% to 16% of the US service members deployed to Afghanistan and Iraq have been affected by PTSD or depression” alone. PTSD is the fourth most common VA disability claim, and multiple mental health conditions rank in the top 20.
Veterans suffering from a service-connected mental illness may be eligible for VA disability benefits. Mental illnesses can affect a person’s behavior, cognitive abilities, and emotions. This can make functioning at home or in the workplace difficult. VA mental health disability benefits help a veteran live a more satisfying life.
This article will discuss how to get VA disability for mental health conditions. Top points include:
- Many mental health conditions are eligible for VA disability compensation—including preexisting conditions, if aggravated—but not illnesses that are genetic or “developmental defects.”
- Getting VA disability compensation for mental health requires proving service connection through direct evidence, presumptions, secondary service connection, or aggravation.
- Many denied mental health VA claims would have benefitted from more lay evidence and C&P exam preparation.
- VA may grant TDIU—the equivalent of 100 percent disability—on the basis of mental health conditions.
NOTE: The Veterans Crisis Line is free, confidential, and available 24/7. Ways to access:
- Dial 988 and pressing 1
- Chat online at https://www.veteranscrisisline.net/get-help-now/chat/
- Send a text message to 838255
What Mental Illnesses are Eligible for VA Disability for Mental Health?
Mental illnesses that VA will consider for service connection include:
- Anxiety (including panic disorder and post-traumatic stress disorder (PTSD))
- Amnesia
- Chronic adjustment disorder
- Cognitive disorders
- Eating disorders (e.g., anorexia and bulimia)
- Mood disorders
- Schizophrenia and other psychotic disorders
- Somatoform disorders (i.e., mental disorders that manifest as unexplained physical ailments)
For any mental health condition to qualify for VA disability compensation, veterans must prove to VA that their disorder is a result of military service.
What Mental Health Conditions Are Not Eligible for VA Disability Benefits?
VA will not grant service connection for mental illnesses that are genetic or “developmental defects.” Examples include:
- Personality Disorders: Military service cannot cause a personality disorder because these types of conditions have lifelong behavioral patterns that do not change.
- Substance Use Disorder: VA does not directly grant service connection for substance use disorder. However, veterans can be service-connected on a secondary basis for disabilities that arise from substance use due to a service-connected condition. For example, a veteran who uses alcohol to cope with symptoms of PTSD and later develops cirrhosis of the liver may be entitled to disability compensation for the liver condition as secondary to PTSD.
- Impulse Control Disorders: These behavioral conditions cause a person to become unable to control their impulses and behaviors, such as angry outbursts. Examples of ICDs include oppositional defiant disorder (ODD) and kleptomania.
- Cognitive Delays and Developmental Disabilities: VA will not consider conditions that are “congenital,” or present since birth. As such, these conditions cannot be considered caused by or aggravated by military service.
Proving Service Connection for VA Disability for Mental Health
Getting VA disability compensation for mental health requires proving service connection through direct evidence, presumptions, secondary service connection, or aggravation.
In most cases, the veteran needs to show that it is “at least as likely as not” (i.e., a 50-50 chance) that military service caused their mental illness or worsened an existing mental health condition.
Direct Service Connection for VA Mental Health Conditions
For veterans to be service-connected for a mental illness on a direct basis, they must prove that their mental health condition “resulted from or was aggravated by their military service.”
Veterans must prove the following:
- A current diagnosis of their condition, and
- An in-service event, injury, or illness, and
- A medical nexus linking the condition to the event.
Examples of evidence that could help prove service connection for mental health disabilities include the following:
- Form DD214 (military discharge papers) provides evidence of military service.
- Service treatment records (i.e., medical records) can show evidence of in-service events, injuries, or illnesses.
- Current medical records—including doctors’ reports and rest results—can show a current diagnosis and impact of the mental health condition.
- VA Form 21-0781, or “Statement in Support of Claimed Mental Health Disorder(s) Due to an In-Service Traumatic Event(s)”
- Lay evidence (see section below).
Presumed Service Connection: Are There Presumptions for Mental Illness?
Some medical conditions are automatically presumed to be service-connected. The veteran must have served at certain places and times and have one or more of the following mental health conditions:
- Psychotic disorders
- Anxiety disorders, such as panic disorder or agoraphobia
- Mood disorders, such as major depression
Note: Some mental health conditions must develop within a year of being discharged to be considered presumptive by VA. For more information on presumptive disability benefits, you can read more from VA itself (PDF).
Secondary Service Connection: Mental Illness Causing or Caused by Other Disabilities
Secondary service connection refers to when a service-connected condition causes another condition to develop. Veterans can receive a disability rating for the new condition. Mental illness may lead to other disabilities and vice versa.
Common service-connected disabilities that may lead to mental health conditions include:
- Diabetes
- Irritable bowel syndrome
- Heart disease
- Thyroid conditions
- Chronic pain
In terms of mental illness leading to other disabilities, some of the most common scenarios include:
- Migraines secondary to depression
- Sleep apnea secondary to depression
- Hypertension secondary to PTSD
Aggravation of Preexisting Mental Health Conditions
If a veteran had a mental illness before their military service, but it was worsened due to their service, then they may still be able to get service connection based on aggravation.
If a service member has any conditions before entry into service, the conditions should be noted on their entrance examination. Otherwise, the presumption of soundness applies, and the veteran is unlikely to qualify for service connection based on aggravation.
Note that VA may attempt to deny service connection for conditions that predate service. Using medical evidence or expert opinions, the veteran must show that:
- Their preexisting condition worsened during service.
- The worsening progression of the preexisting condition is beyond the natural progression of that condition.
Additional Tips for Proving Service Connection for VA Mental Health Disability Claims
At Chisholm Chisholm & Kilpatrick, we have noticed that many denied mental health claims would have benefitted from more lay evidence and C&P exam preparation. If you need assistance developing your appeal, consider contacting us.
How Lay Evidence Can Help a Mental Health VA Disability Claim
Lay evidence is often overlooked as a way to prove service connection, but it can be very important. Lay evidence is personal statements written by someone familiar with the veteran’s situation. Here are a few examples of lay evidence:
- A personal statement: lay evidence written by the veteran detailing their personal experience during and after service.
- A buddy letter: lay evidence written by a fellow service member who witnessed the in-service event.
- A spousal letter: lay evidence detailing the veteran’s daily struggles with their service-related disability and/or the progression of their condition.
- A statement from a coworker: lay evidence demonstrating the veteran’s inability to work due to their service-related condition. This is especially helpful in claims for Total Disability based on Individual Unemployability (TDIU).
Lay evidence can be highly valuable for a mental health claim. For example, CCK may use a letter from a close family member or friend to show the presence of mood swings, nightmares, or anxiety to reinforce medical evidence. Lay evidence can help corroborate stressor events, establish continuity of symptoms, and give evidence of the veteran’s occupational and social impairment.
“VA often takes lay evidence with almost the same weight as medical evidence. So that is something we really look into, especially for a psychiatric condition.” —CCK Supervising Agent Michelle DeTore.
What to Expect at C&P Exams for Mental Health VA Disability Claims
VA uses Compensation and Pension (C&P) examinations to help gather more evidence about a veteran’s mental health condition. It does this before issuing a decision and assigning a rating.
Usually, these exams take place at a VA hospital or with a VA-contracted provider. During these exams, the following typically occurs:
- Evaluation of symptoms: The VA examiner will ask questions about the veteran’s mental health symptoms, which may include questions on their frequency and severity.
- Evaluation of medical history: The veteran’s medical records, and any other relevant information, will be evaluated by the VA examiner.
- Use of DSM-5 Criteria: For mental health conditions, the VA examiner will often assess the veteran using the “Diagnostic and Statistical Manual of Mental Disorders” (DSM-5).
- Disability Benefits Questionnaire (DBQ): The examiner may also utilize a DBQ to help standardize the process. This form includes checkboxes and sections for the examiner to make notes.
A C&P exam should take about 15 to 20 minutes. However, they may range between 5 minutes and several hours. Moreover, VA does not give veterans a copy of their C&P exam unless they request one.
Do I Have to File a Claim for Each of My Mental Disorders Separately?
No. VA does not limit its consideration to the specific mental disorder that the veteran identified within their claim.
After a veteran submits a VA claim for a mental health condition, VA will process the claim as one for any mental health condition. VA will look at:
- The description of the claim
- The veteran’s symptoms
- The information and evidence that the veteran submits
- Any other information and evidence obtained for the claim
For example, a veteran files an initial claim for PTSD. During the processing of their claim, evidence shows that the veteran also has an anxiety disorder. In this scenario, VA is required to consider the anxiety disorder in connection with the initial claim for PTSD. The assigned rating will reflect the severity and impact of both conditions.
How Are Mental Health Disabilities Rated by VA?
VA rates disabilities based on their severity. The more that a veteran’s ability to support themselves has been impacted by their mental health, the higher their VA disability rating.
VA uses the General Rating Formula for Mental Disorders when assigning a disability rating for a service-connected mental disorder. A veteran can receive a VA mental health disability rating of 0, 10, 30, 70, and 100 percent.
Again, VA does not generally consider each of a veteran’s mental health conditions separately. It assesses the impact of all mental health symptoms to assign a single, comprehensive rating.
How to Get TDIU for Mental Illnesses
Mental illnesses can impair a veteran’s ability to work. A mental illness can impact their ability to concentrate, handle the stresses of work, communicate with others, and more. Ultimately, mental health conditions may render a veteran unable to work.
Total Disability based on Individual Unemployability (TDIU) allows veterans who are not rated at 100 percent disabled to be compensated at a 100 percent disability rate anyway due to their conditions preventing them from holding “substantially gainful” employment.”
There are two ways to receive TDIU benefits for mental illness:
- Schedular TDIU—To be eligible for “schedular” TDIU, a veteran must have either 1) a condition rated at least 60 percent, or (2) a combined rating of at least 70 percent and at least one rating of 40 percent or above. Since VA can rate mental health disabilities over 70 percent, schedular TDIU is possible.
- Extraschedular TDIU—Even if a veteran with a mental illness does not meet the rating conditions, they may still qualify for “extraschedular” TDIU if the Director of Compensation Service makes a determination that their service-connected mental health condition is preventing them from holding substantially gainful employment.
Note that mental health does not need to be the only factor causing individual unemployability. A veteran can get TDIU for a combination of mental health and other service-connected disabilities.
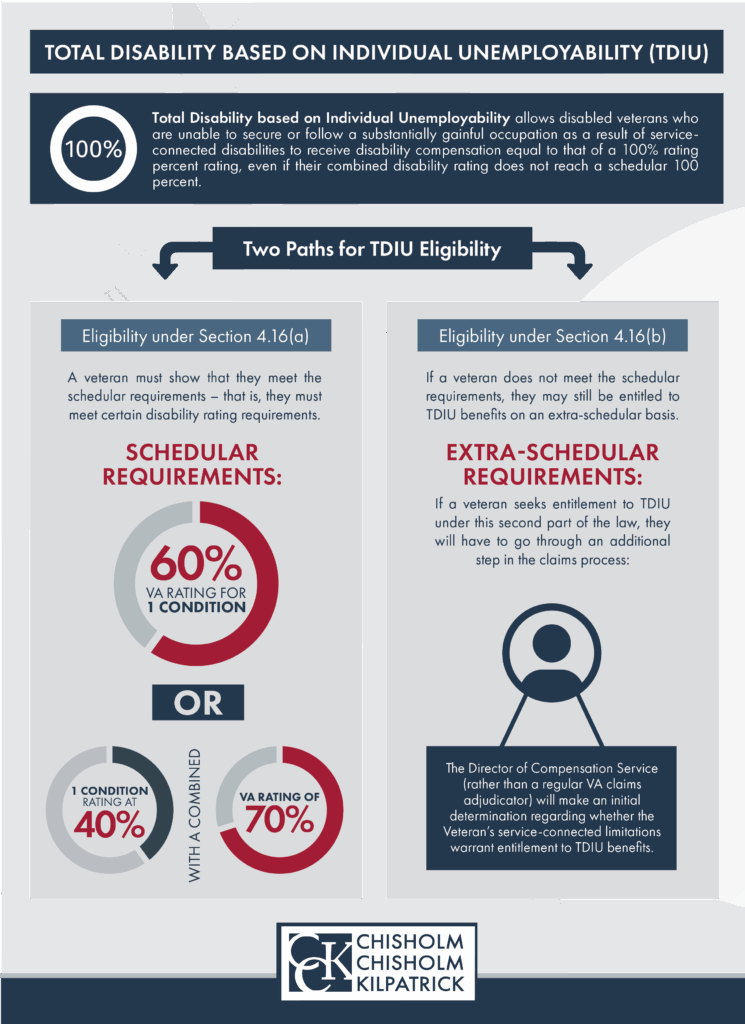
TDIU claims can be highly complex and time-consuming, so utilizing the services of a VA-accredited law firm or agent is recommended.
How to Appeal or Increase Your VA Rating
Veterans may wish to appeal or increase their VA rating in a number of situations, such as:
- VA denied their claim incorrectly
- The veteran believes their rating should be higher
- An existing condition has worsened
- A secondary condition has developed
In these types of situations, veterans have options for appealing or filing supplemental claims.
Denied or Underrated for VA Disability for Mental Health? Call CCK Today
Appeals can be difficult and time-sensitive. Also, veterans have likely already experienced lengthy delays waiting for their initial rating. Therefore, the law permits veterans to hire a VA-accredited law firm or advocate to assist with appeals.
If you are appealing an unfavorable VA decision related to your claim, contact CCK, the most experienced veterans law firm in the U.S. You may call (800) 544-9144 or contact us online.
Share this Post