VA Disability Rating for Spinal Fusion

CCK Law: Our Vital Role in Veterans Law
What is Spinal Fusion?
Generally speaking, spinal fusion is surgery to permanently connect two or more vertebrae in your spine, thereby eliminating motion between them. Spinal fusion involves techniques designed to mimic the normal healing process of broken bones. During spinal fusion, the surgeon places bone or a bonelike material within the space between two spinal vertebrae. In addition, metal plates, screws, and rods may be used to hold the vertebrae together, so they can heal into one solid unit. Spinal fusion may be recommended to treat the following conditions:
- Deformities of the spine – spinal fusion can help correct spinal deformities, such as a sideways curvature of the spine (scoliosis)
- Spinal weakness or instability – your spine may become unstable if there is abnormal or excessive motion between two vertebrae (a common side effect of severe arthritis in the spine); spinal fusion can be used to restore spinal stability in such cases
- Herniated disk – spinal fusion may be used to stabilize the spine after removal of a damaged (i.e., herniated) disk
While spinal fusion is generally a safe, and oftentimes necessary, procedure, there is a risk of complications. Potential complications include: infection, poor wound healing, bleeding, blood clots, injury to blood vessels or nerves in and around the spine, pain at the site from which the bone graft is taken. A hospital stay of two to three days is usually required following spinal fusion.
Depending on the location and extent of your surgery, you may experience some pain and discomfort but the pain can usually be controlled with medications. Importantly, if you exhibit any signs of infection (e.g., redness, tenderness, or swelling; wound drainage; shaking chills; fever higher than 100.4), you should contact your doctor immediately.
Veterans’ Likelihood of Spinal Fusion
Veterans frequently experience back conditions after their time in service. Such back conditions can be due to a specific injury, or general wear and tear due to the physical demands of their time in service. Depending on severity, these conditions can greatly impact a veteran’s ability to perform activities of daily living and work-related responsibilities. It is possible that veterans will require spinal fusion to cope with their back conditions following service. If this is the case, VA disability compensation may be warranted.
Service Connection for Spinal Fusion
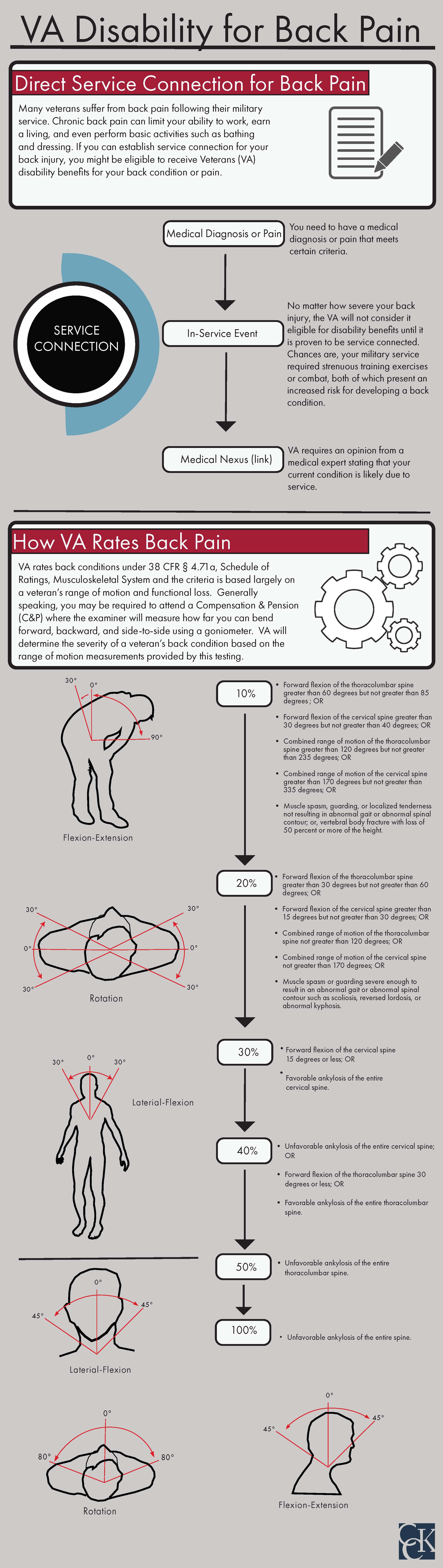
To be granted service connection for spinal fusion, veterans must demonstrate that the spinal fusion was necessary as a result of their time in service. VA generally requires the following three elements to satisfy direct service connection:
- A current diagnosis of a back condition
- An in-service event, injury, or illness
- A medical nexus (i.e. link) between the current, diagnosed back condition and the in-service event, injury, or illness
In this case, the first element of service connection may be satisfied with medical documentation from a healthcare professional indicating that spinal fusion is necessary as a result of the veteran’s back pain or condition. The most important element is the medical nexus in which either a VA healthcare provider or private doctor or medical professional, opines that the veteran’s spinal fusion is at least as likely as not due to their time in service.
How Does VA Rate Spinal Fusion?
VA rates spinal fusion according to 38 CFR § 4.71a, Schedule of Ratings, Musculoskeletal System (Diagnostic Code 5241) and the criteria is based largely on a veteran’s range of motion. Specifically, VA uses the General Rating Formula for Diseases and Injuries of the Spine as follows:
- 100% – unfavorable ankylosis of the entire spine
- 50% – unfavorable ankylosis of the entire thoracolumbar spine
- 40% – unfavorable ankylosis of the entire cervical spine; or, forward flexion of the thoracolumbar spine 30 degrees or less; or, favorable ankylosis of the entire thoracolumbar spine
- 30% – forward flexion of the cervical spine 15 degrees or less; or, favorable ankylosis of the entire cervical spine
- 20% – forward flexion of the thoracolumbar spine greater than 30 degrees but not greater than 60 degrees; or, forward flexion of the cervical spine greater than 15 degrees but not greater than 30 degrees; or, the combined range of motion of the thoracolumbar spine not greater than 120 degrees; or, the combined range of motion of the cervical spine not greater than 170 degrees; or, muscle spasm or guarding severe enough to result in an abnormal gait or abnormal spinal contour such as scoliosis, reversed lordosis, or abnormal kyphosis
- 10% – forward flexion of the thoracolumbar spine greater than 60 degrees but not greater than 85 degrees; or, forward flexion of the cervical spine greater than 30 degrees but not greater than 40 degrees; or, combined range of motion of the thoracolumbar spine greater than 120 degrees but not greater than 235 degrees; or, combined range of motion of the cervical spine greater than 170 degrees but not greater than 335 degrees; or, muscle spasm, guarding, or localized tenderness not resulting in abnormal gait or abnormal spinal contour; or, vertebral body facture with loss of 50 percent or more of the height
In addition to the range of motion measurements outlined above, VA should also address functional loss and the presence of flare-ups.

Functional Loss
C&P examiners and rating adjudicators should also take into account the functional loss caused by the veteran’s spinal fusion, as evidenced by pain during motion. For example, a veteran might be able to bend forward 85 degrees, but starts to experience pain at 55 degrees. In this case, the veteran should receive a disability rating that is consistent with both the range of motion measurements and the functional limitations caused by their back pain.
Flare-Ups
If veterans experience flare-ups of back pain due to spinal fusion, they may be eligible for a higher disability rating. For example, a veteran is receiving a 10 percent disability rating. On most days, the veteran is unable to bend forward more than 60 degrees. However, when experiencing a flare-up, the veteran is unable to bend forward more than 30 degrees. Therefore, during the flare-up the veteran’s spinal fusion becomes much more disabling than 10 percent. As such, VA should assign a disability rating in accordance with this additional loss. In a 2017 Court of Appeals for Veterans Claims (CAVC) case, Sharp v. Shulkin, the Court decided that examiners must offer an opinion on how the veteran could be functionally limited during a flare-up, even if the examination is not being performed during a flare-up. If an examiner fails to do so, then the examination is inadequate for VA rating purposes and a new examination may be warranted.
Overall, VA’s consideration of functional loss and flare-ups accounts for how a veteran’s spinal fusion actually impacts their daily life, making up for the otherwise very mechanical application of the rating schedule.
About the Author
Share this Post