TMJ: VA Disability Claims, Ratings, and Compensation

CCK Law: Our Vital Role in Veterans Law
Temporomandibular joint dysfunction, also known as TMJ or TMD, is a disorder of the joint that connects the jawbone to the skull. Frustrating and painful for those it affects, severe enough TMJ can interfere with a veteran’s ability to speak, eat, or even breathe.
If you are a veteran suffering from service-connected TMJ, then you may be entitled to compensation from the Department of Veterans Affairs (VA). This article will guide you through the disability claims process to help you earn a TMJ VA rating and any potential monthly payments and VA benefits.
Key points of this article include:
- TMJ has many potential causes, including trauma to the head or jaw, arthritis, bruxism, and more. Several of these conditions can have a root cause stemming from military service, which has led to TMJ being a well-known disorder amongst veterans.
- It is possible for veterans to pursue secondary service connection for TMJ through an existing PTSD diagnosis. PTSD and other psychological disorders often cause clenching of the jaw, which can wear away at the joint over time and trigger TMJ to develop.
- Typically, TMJ VA ratings are based on the results of an interincisal opening test, which measures how wide a veteran can open their mouth. This test may be conducted by VA during the veteran’s Compensation & Pension (C&P) exam.
What is Temporomandibular Joint Dysfunction (TMJ)?
The temporomandibular joint is a joint on either side of the jaw. This joint acts like a sliding hinge, connecting a veteran’s jawbone to their skull. Matt Fusco, an Accredited Claims Agent at CCK Law, provides a definition for the dysfunction of this joint:
“Another disability veterans may receive a rating for is temporomandibular disorder, also called TMJ or TMD. This is a condition where the jaw muscles and nerves will frequently cause chronic facial pain.”
In most cases, the pain and discomfort associated with TMJ dysfunction are temporary and can be relieved with self-managed care or nonsurgical treatments.
Surgery is typically a last resort after conservative measures have failed, but some people with TMJ disorders may benefit from surgical treatments. Common signs and symptoms of TMJ dysfunction may include the following:
- Pain or tenderness of the jaw
- Pain in one or both of the temporomandibular joints
- Aching pain in and around the ear
- Difficulty chewing or pain while chewing
- Headaches
- Aching facial pain
- Locking of the joint, making it difficult to open or close the mouth
- Clicking sound or grating sensation when opening the mouth or chewing
- Trouble speaking, breathing, or eating
- Neck pain
In addition to these symptoms, studies show that tinnitus can also be a symptom of TMJ. This is likely due to the close proximity of the jaw to the ear’s structures, as well as the nerve pathways they share. If a veteran’s tinnitus changes pitch, frequency, or intensity as they move their jaw, it is possible their tinnitus is somehow related to their TMJ.
Why Are Veterans Prone to TMJ?
Military service can be harsh on the body, causing wear and tear that contributes to chronic conditions later in a veteran’s life. Some common causes of TMJ among veterans include:
- Facial injury – Over the course of their service, some veterans may be exposed to explosions or falls that cause significant facial injury. Painful TMJ dysfunction can occur if these injuries cause the shock-absorbing disk in the jaw to erode or move out of its proper alignment.
- Arthritis – Arthritis is a common source of pain for many veterans, with the physical strain of military life often contributing to osteoarthritis in certain joints of the body. A veteran suffering from arthritis of the jaw may eventually develop TMJ.
- Psychological disorders – Studies show that mental disorders like post-traumatic stress disorder (PTSD) can lead a veteran to frequently clench their jaw or grind their teeth, a condition called bruxism. Over time, this can put stress on the joints of the jaw and cause TMJ.
In addition to these causes, certain connective tissue disorders may also be the reason a veteran develops TMJ. However, just as often, the cause of a veteran’s TMJ dysfunction can be unclear.
Watch CCK Law’s VA-accredited advocates discuss VA Disability Ratings for Dental Disabilities:
How Do I Prove Service Connection for a TMJ VA Rating?
Prior to receiving VA disability benefits for TMJ, veterans must establish service connection—that is, they must prove their TMJ is somehow a result of their military service. There are multiple types of service connection. However, the following two types are most common in claims for TMJ:
Direct Service Connection for TMJ
Direct service connection is when a veteran has a condition that can be directly linked back to their military service, like an injury or exposure they suffered while in uniform. CCK Law partner Robert Chisholm describes the three components that veterans must demonstrate to VA to establish direct service connection:
“In order to qualify for VA benefits for dental disabilities, veterans must have:
(1) a current diagnosis of a dental or oral condition [like TMJ] by a medical professional;
(2) evidence of an in-service event, injury, or illness; and
(3) a medical nexus between the in-service event and the resulting dental disability.”
For example:
- Say a veteran is diagnosed with TMJ by their doctor.
- An in-service event they could link to their diagnosis could be an IED blast, as TMJ is associated as being a chronic pain disorder linked to IED-related conditions. Specifically, the IED blast may result in severe injury to the jaw or the muscles near the head and neck, thereby causing TMJ.
- Finally, the veteran must have a doctor provide their opinion that the veteran’s TMJ is “at least as likely as not” due to their service.
Secondary Service Connection for TMJ
Secondary service connection is warranted when a veteran has a primary service-connected condition that then causes or aggravates a secondary condition. In other words, veterans may be awarded secondary service connection for TMJ if they can prove it is the result of a separate, service-connected condition.
For example:
- Say a veteran is diagnosed with PTSD as a result of a battle they were involved in during their military service. VA recognizes that the veteran’s PTSD is service connected, and assigns the veteran a PTSD disability rating.
- Over time, the stress and anxiety brought on by the PTSD cause the veteran to frequently clench their jaw and grind their teeth. This puts strain on the veteran’s temporomandibular joint, and they eventually develop TMJ because of it. The veteran’s doctor also provides their medical opinion supporting this sequence of events.
- In this case, the veteran may be able to file a claim for TMJ secondary to PTSD, since the root cause of the veteran’s TMJ was determined by a doctor to be their already service-connected PTSD. If the veteran’s claim is successful, they could earn a TMJ VA rating and compensation.
What Evidence to Submit for a TMJ VA Rating
When applying for a TMJ VA rating, the strength of a veteran’s claim often hinges on the type and quality of evidence they present. Building a persuasive case usually requires submitting several different kinds of documentation:
- Service records – These help demonstrate a direct connection between military service and the veteran’s TMJ. Useful documents could include incident reports describing in-service accidents the veteran may have suffered, as well as medical reports detailing relevant injury or trauma to the veteran’s jaw.
- Medical evidence and opinions – Medical evidence is often essential to help a veteran win their TMJ case. For instance, if the veteran’s doctor offers their official opinion that the veteran’s TMJ was caused by in-service trauma they suffered, this could serve as a nexus and help the veteran prove service connection.
- Lay evidence – In addition to these records, veterans may also provide lay evidence—personal observations from family, friends, or coworkers. Although not as authoritative as official documentation, such statements can paint a clearer picture of how TMJ affects the veteran’s day-to-day life and add valuable context to the claim.
It is also worth noting that veterans are not expected to handle the actual evidence gathering entirely on their own. VA actually has a “duty to assist” which requires it to make a reasonable effort to locate and collect relevant records, as long as it is made aware that the records exist.
Compensation & Pension (C&P) Exams for TMJ
A Compensation & Pension (C&P) exam is a medical examination carried out either by a VA clinician or a contractor authorized by VA. This evaluation plays a key role in the claims process because it helps VA decide whether a veteran’s health condition is linked to their time in service. The results also give VA the information needed to assign a disability rating once service connection has been established.
When it comes to TMJ, veterans should typically expect the following from their C&P exam:
- An interincisal test is one of the primary methods by which VA examiners determine the severity of a veteran’s TMJ. This test measures the vertical distance by which a veteran can open their mouth. The smaller the vertical distance, the higher a veteran’s TMJ VA rating is likely to be.
- A TMJ lateral excursion test is another test the VA examiner might conduct on the veteran. This test measures a veteran’s ability to move their jaw side to side.
- A questionnaire portion is another part of the C&P exam that veterans should prepare for. Typically, this portion will have the VA examiner ask the veteran questions about any potential in-service events that could have caused their condition. They will likely also ask about how the veteran’s TMJ affects their employability and quality of life, such as whether the veteran is limited to eating mechanically altered foods due to the pain caused by the disorder.
After the C&P exam is conducted and service connection is established, the veteran’s test results will contribute significantly to their overall TMJ VA rating.
How VA Rates TMJ for Disability Compensation
VA rates veterans at 10, 20, 30, 40, or 50 percent for TMJ, depending on its severity and how much it limits the range of motion of their jaw.
The rating criteria for TMJ fall under 38 CFR § 4.150, Schedule of Ratings – Dental and Oral Conditions, Diagnostic Code 9905. Essentially, these rating criteria are based on limited motion of the joint and the ability to eat regular or mechanically altered food.
Veterans with TMJ may have a limited range of motion when (1) opening and closing the jaw and (2) moving the jaw side-to-side. Only one direction of motion will be rated. If the veteran experiences limitation of motion in both directions, then the one that will give the highest disability rating is used.
Mechanically altered foods include liquid, blended, chopped, pureed, ground, mashed, soft, and semisolid foods. Importantly, it is not enough for veterans to report that they eat mechanically altered foods. Instead, a treating physician must record that the veteran’s condition requires them to eat only mechanically altered foods to receive a disability rating under that specific criterion.
The rating criteria for TMJ are broken down as follows:
Interincisal Range of Motion (opening and closing the jaw)
- 0 to 10 millimeters (mm) of maximum unassisted vertical opening:
- 50% – with dietary restrictions to all mechanically altered foods
- 40% – without dietary restrictions to mechanically altered foods
- 11 to 20 mm of maximum unassisted vertical opening:
- 40% – with dietary restrictions to all mechanically altered foods
- 30% – without dietary restrictions to mechanically altered foods
- 21 to 29 mm of maximum unassisted vertical opening:
- 40% – with dietary restrictions to full liquid and pureed foods
- 30% – with dietary restrictions to soft and semi-solid foods
- 20% – without dietary restrictions to mechanically altered foods
- 30 to 34 mm of maximum unassisted vertical opening
- 30% – with dietary restrictions to full liquid and pureed foods
- 20% – with dietary restrictions to soft and semi-solid foods
- 10% – without dietary restrictions to mechanically altered foods
Importantly, for VA compensation purposes, the normal maximum unassisted range of vertical jaw opening is from 35 to 50 mm.
Lateral Excursion Range of Motion (moving the jaw side-to-side)
- 10% – 0 to 4 mm
How to Apply for a VA Rating for TMJ/TMD
- If a veteran needs more time to gather evidence for their TMJ claim, they can start by submitting VA Form 21-0966. This form notifies VA of the veteran’s intent to file a claim within the next year. The date VA receives this form will then count as the effective date of the veteran’s claim, potentially granting the veteran higher retroactive awards if their claim is successful.
- When ready to start their claim, a veteran must fill out VA Form 21-526EZ.
- The veteran must submit the form to VA in one of the following ways:
- Online – through VA.gov
- By mail – send to the Department of Veterans Affairs, Evidence Intake Center, PO Box 4444 in Janesville, WI 53547-4444
- In person – by bringing the form to the nearest VA Regional Office
- With a legal representative – complete the form with the help of a Veterans Service Organization (VSO), or a VA-accredited agent or attorney
- Generally, submitting the form online through VA.gov will be the quickest way to do so, and may even help the veteran establish an earlier effective date for the purpose of earning greater retroactive benefits.
VA Compensation for TMJ
Veterans with a TMJ rating of 10 percent or higher may be eligible for financial benefits from VA, with their monthly compensation increasing as their TMJ rating percentage goes up.
As of 2026, the VA disability rate benefit amounts are as follows:
- 0 percent disability rating: $0.00 per month
- 10 percent disability rating: $180.42 per month
- 20 percent disability rating: $356.66 per month
- 30 percent disability rating: $552.47 per month
- 40 percent disability rating: $795.84 per month
- 50 percent disability rating: $1,132.90 per month
- 60 percent disability rating: $1,435.02 per month
- 70 percent disability rating: $1,808.45 per month
- 80 percent disability rating: $2,102.15 per month
- 90 percent disability rating: $2,362.30 per month
- 100 percent disability rating: $3,938.58 per month
Veterans who have dependents—like a spouse, children, or other qualifying family members—may also be entitled to additional monthly compensation, which can raise the total amount they receive.
In addition to financial compensation, VA offers a variety of additional benefits to veterans depending on the disability rating percentage they earn for TMJ. Some of these benefits include monthly financial compensation, no-cost health care, money for education and training, a hiring preference for federal jobs, and more.
Special Monthly Compensation (SMC) for TMJ
Special Monthly Compensation (SMC) is an additional form of VA benefit available to veterans with severe disabilities or complex medical needs. Unlike standard disability payments, these enhanced rates are intended to address circumstances where extra financial support is necessary.
In certain situations, TMJ can cause long-term complications or contribute to more serious health problems. For example, if the condition causes a veteran to require assistance to conduct the activities of daily life, VA may award SMC as added compensation.
Can I Get Total Disability for TMJ?
Yes, veterans can qualify for total disability benefits due to TMJ. However, this is unlikely to happen if a veteran is suffering from TMJ alone.
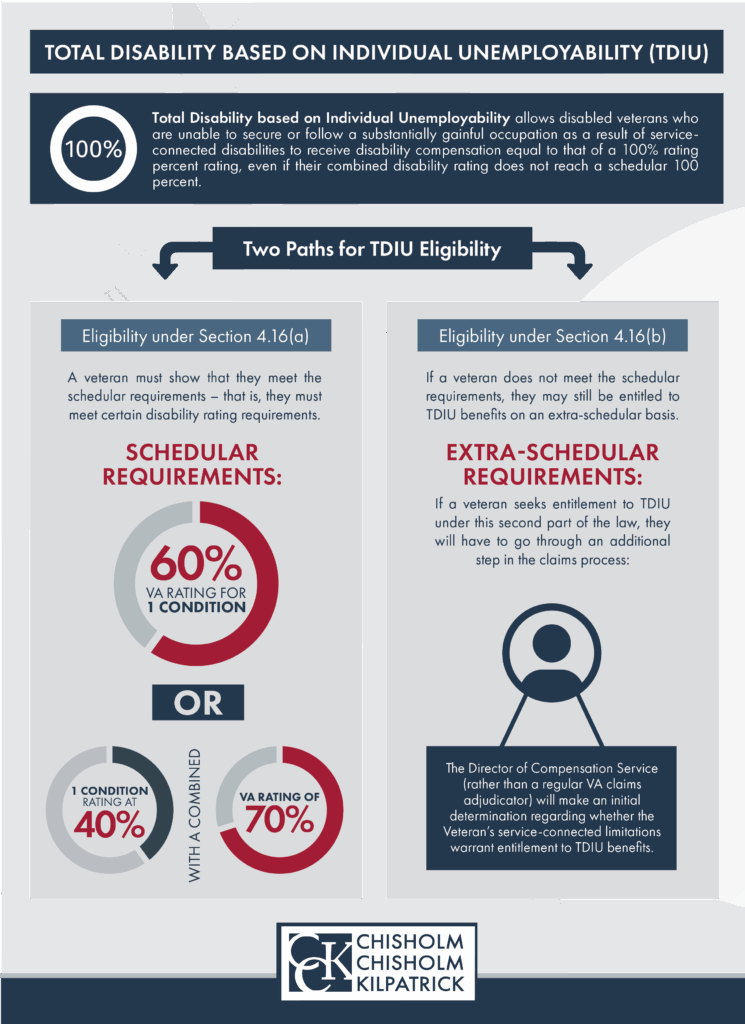
Through Total Disability based on Individual Unemployability (TDIU), veterans can earn compensation at the 100 percent level, even if their disability is not rated at 100 percent. This benefit is designed for veterans whose service-connected conditions prevent them from maintaining substantially gainful employment.
However, TDIU would be difficult to earn for TMJ. This is because TMJ by itself can only grant a veteran a maximum 50 percent disability rating, which is not high enough to qualify for TDIU.
To qualify for TDIU, a veteran would need either an additional service-connected condition to grant them a higher combined rating or they could apply for extraschedular TDIU. Extraschedular TDIU can be difficult to prove, particularly without the help of a VA-accredited advocate.
Want to Appeal Your TMJ VA Rating? Contact CCK Law
Did VA deny your disability claim for TMJ? If so, the dedicated team at Chisholm Chisholm & Kilpatrick might be able to assist. The VA-accredited attorneys at CCK Law have represented thousands of veterans before VA and have helped recover over $1 billion in wrongfully denied compensation.
Call CCK Law today at (800) 544-9144 or contact us online for a free case evaluation with a member of our team.
About the Author
Share this Post
