Fatty Liver Disease and VA Disability Ratings
CCK Law: Our Vital Role in Veterans Law
What is Fatty Liver Disease?
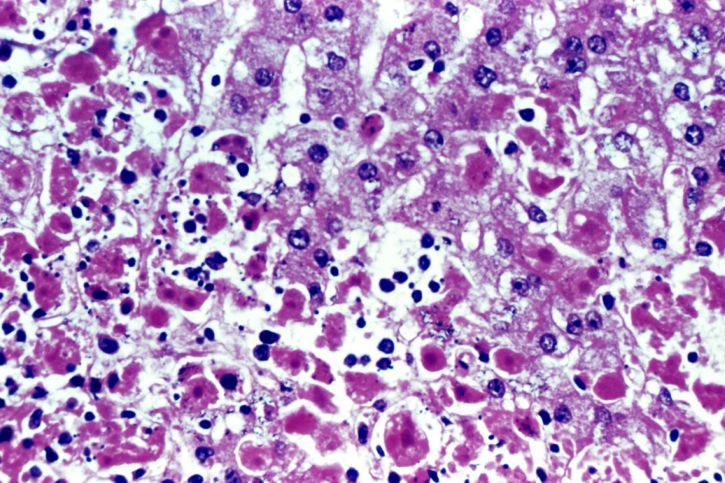
The liver is the largest organ inside the body and aids in digestion, energy storage, and removal of toxins. Fatty liver disease is a condition in which fat builds up in your liver. There are two main types:
Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease is a type of fatty liver disease that is not related to heavy alcohol use. It includes two further subtypes:
- Simple fatty liver – you have fat in your liver but little or no inflammation or liver cell damage. This subtype of nonalcoholic fatty liver disease does not usually get severe enough to cause liver damage or complications.
- Nonalcoholic steatohepatitis – you have inflammation and liver cell damage, as well as fat in your liver. Here, inflammation and liver cell damage can cause scarring of the liver. This subtype may lead to cirrhosis or liver cancer.
Alcoholic Fatty Liver Disease
Alcoholic fatty liver disease is due to heavy alcohol use and consumption. Specifically, the body’s process of breaking down alcohol can generate harmful substances, which then damage liver cells, promote inflammation, and weaken your body’s natural defenses. If alcoholic fatty liver disease progresses, it typically results in alcoholic hepatitis and cirrhosis.
Service Members and Nonalcoholic Fatty Liver Disease
Between 2000 and 2017, the incidence of nonalcoholic fatty liver disease among active duty military service members has increased from 12.6 cases per 100,000 person per year to 152.8 cases. The overall rate of incidence among male service members was more than 1.5 times the rate among female service members. Furthermore, overall incidence rates increased with advancing age and were highest among military personnel 50 years or older. This is significant because service members with severe nonalcoholic fatty liver disease resulting in impaired liver function are unable to perform their military duties and are disqualified from service. Moreover, the repercussions of this increase in incidence could be serious and have a profound effect on both VA and the Veterans Health Administration.
Service Connection for Fatty Liver
To receive service connection for fatty liver disease, veterans must demonstrate the following:
- A current diagnosis of fatty liver disease;
- An in-service event, injury, or illness related to the fatty liver disease; and
- A medical nexus linking the current diagnosis of fatty liver disease to the in-service event, injury, or illness
For example, a veteran underwent a medical examination during service and was noted to have high cholesterol. The medical personnel prescribed an oral medication used to help lower bad cholesterol and fats and raise good cholesterol in the blood. The veteran then developed fatty liver disease as a result of taking this medication. Here, the veteran may be qualified for service connection on the basis that their condition resulted from the cholesterol medication prescribed during service. Most likely the veteran would need to attend a Compensation & Pension examination in order for a VA examiner to provide a nexus opinion.
How VA Rates Fatty Liver Disease
Once service connection is established, VA will provide a disability rating depending on the severity of the condition. VA rates fatty liver disease under 38 CFR § 4.114, Schedule of Ratings – Digestive System, Diagnostic Code (DC) 7345. This DC applies to any chronic liver disease that does not include cirrhosis and the evaluations are as follows:
- 100 percent – “Progressive chronic liver disease requiring use of both parenteral antiviral therapy (direct antiviral agents), and parenteral immunomodulatory therapy (interferon and other); and for six months following discontinuance of treatment”
- 60 percent – “Progressive chronic liver disease requiring continuous medication and causing substantial weight loss and at least two of the following:
- daily fatigue
- malaise
- anorexia
- hepatomegaly
- pruritus
- arthralgia”
- 40 percent – “Progressive chronic liver disease requiring continuous medication and causing minor weight loss and at least two of the following:
- daily fatigue
- malaise,
- anorexia
- hepatomegaly
- pruritus
- arthralgia
- 20 percent – “Chronic liver disease with at least one of the following:
- intermittent fatigue
- malaise,
- anorexia
- hepatomegaly
- pruritus”
- 0 percent – “Previous history of liver disease, currently asymptomatic”
About the Author
Share this Post
