Fatty Liver Disease and VA Disability Ratings
CCK Law: Our Vital Role in Veterans Law
What Is Fatty Liver Disease?
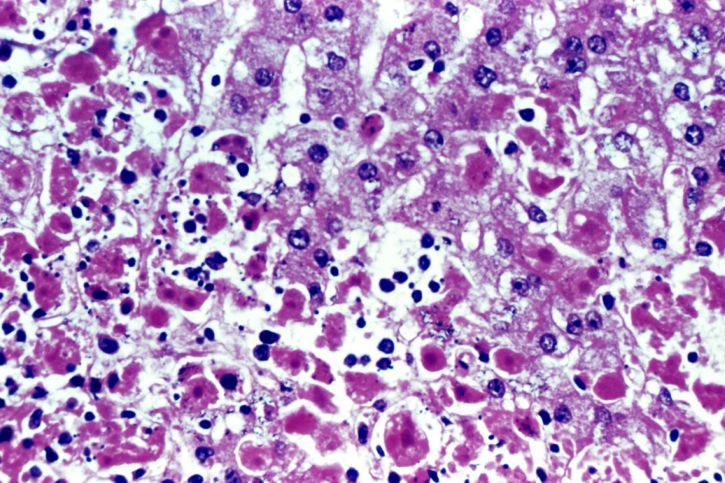
Fatty liver disease is a condition in which fat builds up in the liver, potentially leading to liver damage or the development of more severe diseases. The liver is the largest organ inside the body and aids in digestion, energy storage, and removal of toxins. When it is damaged, it can have serious effects on a veteran’s health. There are two main types of fatty liver disease:
Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease, also called metabolic dysfunction-associated steatotic liver disease (MASLD), is a type of fatty liver disease that is not related to heavy alcohol use. It includes two further subtypes:
- Simple fatty liver – you have fat in your liver but little or no inflammation or liver cell damage. This subtype of nonalcoholic fatty liver disease does not usually get severe enough to cause liver damage or complications.
- Nonalcoholic steatohepatitis – you have inflammation and liver cell damage, as well as fat in your liver. Here, inflammation and liver cell damage can cause scarring of the liver. This subtype may lead to cirrhosis or liver cancer.
Alcoholic Fatty Liver Disease
Alcoholic fatty liver disease (AFLD) is due to heavy alcohol use and consumption. Specifically, the body’s process of breaking down alcohol can generate harmful substances, which then damage liver cells, promote inflammation, and weaken your body’s natural defenses. If alcoholic fatty liver disease progresses, it typically results in alcoholic hepatitis and cirrhosis.

Is Nonalcoholic Fatty Liver Disease Common Among Veterans?
Yes, nonalcoholic fatty liver disease is fairly common amongst veterans. One 2023 study determined that, of a sample population of veterans receiving primary care through VA, about 40 percent could be diagnosed with nonalcoholic fatty liver disease, with ten percent suffering from some sort of liver scarring or damage. The study hypothesizes that these high rates of liver disease are due to the prevalence of conditions like diabetes and obesity among veterans.
Additionally, rates of nonalcoholic fatty liver disease seem to be rising among servicemembers. One 2019 study concluded that, between 2000 and 2017, the incidence of nonalcoholic fatty liver disease among active duty military service members increased from 12.6 cases per 100,000 person per year to 152.8 cases. The overall rate of incidence among male service members was more than 1.5 times the rate among female service members. Furthermore, overall incidence rates increased with advancing age and were highest among military personnel 50 years or older.
This is significant because service members with severe nonalcoholic fatty liver disease resulting in impaired liver function are unable to perform their military duties and are disqualified from service. Moreover, the repercussions of this increase in incidence could be serious and have a profound effect on both VA and the Veterans Health Administration.
How Do I Prove Service Connection for Fatty Liver Disease?
To prove service connection for fatty liver disease, veterans must provide evidence of the following to VA:
- A current diagnosis of fatty liver disease;
- An in-service event, injury, or illness related to the fatty liver disease; and
- A medical nexus linking the current diagnosis of fatty liver disease to the in-service event, injury, or illness
An example of this in action might resemble the following:
- Say a veteran underwent a medical examination during service and was noted to have high cholesterol. The medical personnel then prescribed the veteran an oral medication used to help lower bad cholesterol and fats and raise good cholesterol in the blood.
- However, the medication had an adverse effect on the veteran, eventually causing them to develop fatty liver disease, for which they receive an official diagnosis from their doctor.
- Here, the veteran may be qualified for service connection on the basis that their condition resulted from the cholesterol medication prescribed during service, which would count as an in-service event.
- Finally, the veteran would likely need to attend a Compensation & Pension examination in order for a VA examiner to provide a nexus opinion.
How Does VA Rate Fatty Liver Disease?
Once service connection is established, VA will provide a disability rating depending on the severity of the condition. VA rates fatty liver disease under 38 CFR § 4.114, Schedule of Ratings – Digestive System, Diagnostic Code (DC) 7345. This DC applies to any chronic liver disease that does not include cirrhosis and the evaluations are as follows:
- 100 percent – “Progressive chronic liver disease requiring use of both parenteral antiviral therapy (direct antiviral agents), and parenteral immunomodulatory therapy (interferon and other); and for six months following discontinuance of treatment”
- 60 percent – “Progressive chronic liver disease requiring continuous medication and causing substantial weight loss and at least two of the following:
- daily fatigue
- malaise
- anorexia
- hepatomegaly
- pruritus
- arthralgia”
- 40 percent – “Progressive chronic liver disease requiring continuous medication and causing minor weight loss and at least two of the following:
- daily fatigue
- malaise,
- anorexia
- hepatomegaly
- pruritus
- arthralgia
- 20 percent – “Chronic liver disease with at least one of the following:
- intermittent fatigue
- malaise,
- anorexia
- hepatomegaly
- pruritus”
- 0 percent – “Previous history of liver disease, currently asymptomatic”
VA Deny Your Liver Disease Claim? Contact CCK Law
If VA denied your claim for fatty liver disease, then the attorneys at Chisholm Chisholm & Kilpatrick may be able to assist. CCK Law is the leading veterans law firm in the nation, having represented over 18,000 veterans and dependents before VA and helping to secure over $1 billion in wrongfully denied compensation.
Call CCK Law today at (800) 544-9144 or contact us online for a free evaluation of your case.
About the Author
Share this Post
