Evidence of DNA Damage Found in Veterans With Gulf War Illness
CCK Law: Our Vital Role in Veterans Law
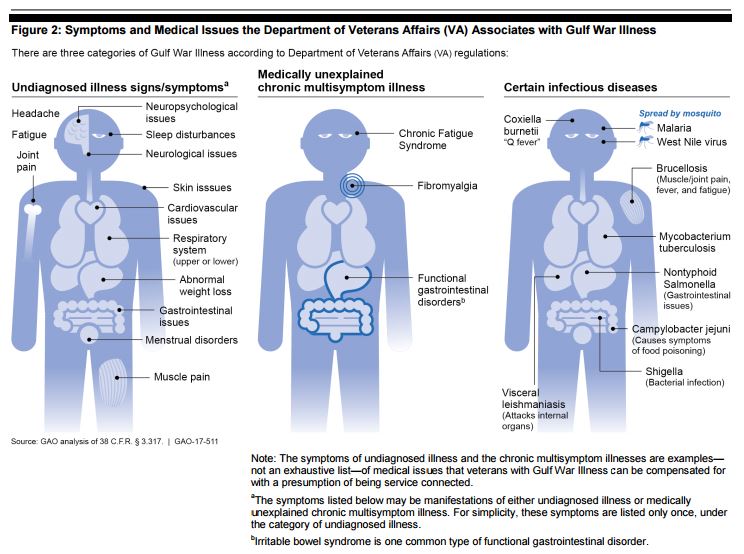
For decades, doctors and researchers have been perplexed by the cluster of illnesses referred to as Gulf War Illness or Gulf War Syndrome. The Department of Veterans Affairs (VA) has even resorted to calling the complex sets of symptoms “Undiagnosed illness” and “Medically Unexplained Chronic Multi-Symptom Illness.” But recent research may make these terms obsolete.
Researchers from the VA and Rutgers University say they have found the “first direct biological evidence” of DNA damage in veterans with Gulf War Illness (GWI), a discovery which could lead to a more complete understanding of the illness and promising new treatment options.
Why look at DNA damage to study Gulf War Illness?
The study focused on mitochondrial DNA (mtDNA)—DNA found in cellular structures (called mitochondria) that produce energy in the body. Researchers were looking for lesions in the mtDNA that would give a direct measure of DNA damage. They also counted the number of mtDNA copies, which reflects the body’s response to the damage.
According to lead researcher Dr. Mike Falvo, both lesion frequency and the number of mtDNA copies are known to change in response to environmental toxins. And most of the leading theories on the cause(s) of Gulf War Illness cite exposure to powerful toxins like sarin gas (nerve gas), smoke from burning oil wells, and even depleted uranium.
Additionally, patients with mitochondrial dysfunction (which is consistent with mtDNA damage) have symptoms involving multiple organ systems, primarily nerves and muscles. Similarly, veterans experiencing Gulf War Illness report a wide range of symptoms all over the body, including chronic fatigue, fibromyalgia (widespread muscle pain), and issues with their gastrointestinal, respiratory, cardiovascular, and neurological systems.
Dr. Falvo, after joining the New Jersey VA medical system in 2010, learned of the symptoms Gulf War veterans. “To me, that sounded awfully consistent with the symptoms of mitochondrial disorders,” he said, according to EurekAlert.org. “After reviewing the literature, I realized at that time there was no published study on GWI that investigated whether mitochondrial dysfunction contributed to symptoms.”
The Findings
Researchers collected blood samples from 21 veterans with Gulf War Illness and seven controls. The control group included three veterans without GWI and four non-veterans. In blood tests, researchers observed significantly more lesions and more mitochondrial DNA (i.e. extra copies of genes) in veterans with Gulf War Illness than they did in the control group without the illness.
Though everyone experiences some level of mtDNA damage due to aging and environmental exposures like air pollution, the veterans with GWI had 20 percent greater mtDNA damage compared to the control group.
Falvo and his team were interested mainly in mtDNA, but they also looked at nuclear DNA, another important factor in mitochondrial health. They found that the veterans with GWI also had more damage to their nuclear DNA than the control group. However, the difference in damage levels between the group reportedly did not reach “statistical significance.” Nuclear DNA damage is a major cause of cancer, neurodegeneration, mitochondrial dysfunction, and other diseases.
Hope for Better Treatment
In 2014, a study of 46 veterans with GWI found promising results for the nutritional supplement coenzyme Q10 (CoQ10) as a way to address their fatigue, which is now believed to be caused by mitochondrial dysfunction. CoQ10 is thought to promote healthy mitochondria and, as an antioxidant, it helps to remove potentially damaging toxins in the body. Some researchers think CoQ10 could even serve to repair already-damaged mitochondria.
VA recently launched a three-year trial to see if treatment with ubiquinol, a form of CoQ10, improves the physical function and fatigability of veterans suffering from Gulf War Illness. In another study by the South Florida Veterans Affairs Foundation for Research and Education, a nonprofit group that supports VA research, researchers are delving into the biological mechanisms of CoQ10 treatment by looking for changes in “biomarkers.” These biomarkers include inflammatory cytokines, which are secreted by certain cells in the immune system (another system thought to be affected by GWI); and natual killer (NK) cells, which play a major role in the hosting and rejection of tumors and virally infected cells.
Dr. Falvo also hopes to expand his research on mitochondrial DNA damage in veterans with Gulf War Illness. With funding from the DoD and a partnership with researchers from Duke University, he is seeking to study 150 veterans with and without GWI.
“We need to be sure our findings are robust,” Falvo said, according to EurekAlert.org. “For us, that means confirming the present results but also investigating what might be contributing to mitochondrial DNA damage or its lack of repair.”
Source: The medical journal PLOS One (September 2017), via EurekAlert.org
RELATED READ: VA denies over 80% of Gulf War claims, report finds
About the Author
Share this Post
