“Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans” (2019)
CCK Law: Our Vital Role in Veterans Law
In April 2019, the Health and Medicine Division (formally known as the Institute of Medicine) of the National Academy of Sciences, Engineering, and Medicine released its report “Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans.”
Overview of the VA Disability Compensation Process
The Veterans Benefits Administration (VBA) provides disability compensation to veterans with a service-connected condition. Disability compensation is a tax-free monetary benefit paid to veterans with disabilities that are the result of a disease or injury incurred or aggravated during active military service. Veterans must first submit claims for their conditions and be granted service connection to then be assigned an evaluation according to the Veterans Affairs Schedule for Rating Disabilities (VASRD). The veterans’ disability ratings, or combined disability ratings (if more than one service-connected condition) determine the amount of monthly compensation they receive.
About the Report
A committee was formed in response to Public Law 114-315 passed in December 2016, which required that VA contract with the National Academies to provide an independent review of the process by which VA assesses impairments resulting from traumatic brain injury (TBI) for purposes of awarding VA disability compensation. In its report, the committee was instructed to make the following determinations:
- A determination of the adequacy of the tools and protocols used by VA to provide examinations for TBI; and
- A determination of which credentials are necessary for health care specialists and providers to perform such portions of such examinations that relate to an assessment of all disabling effects of TBI.
Upon making such determinations, the committee was required to include the following in its final report:
- Findings with respect to the comprehensive review based on the above; and
- Recommendations for legislative or administrative action for improving the adjudication of veterans’ claims seeking entitlement to compensation for all impairments arising from TBI
Ultimately, the committee provided recommendations to VA related to the healthcare specialists who diagnose TBI, the adequacy of the tools used by VA to provide clinical examinations and disability ratings for TBI residuals (i.e. the Disability Benefits Questionnaire and the VASRD), and the overall adjudication process.
Traumatic Brain Injury (TBI)
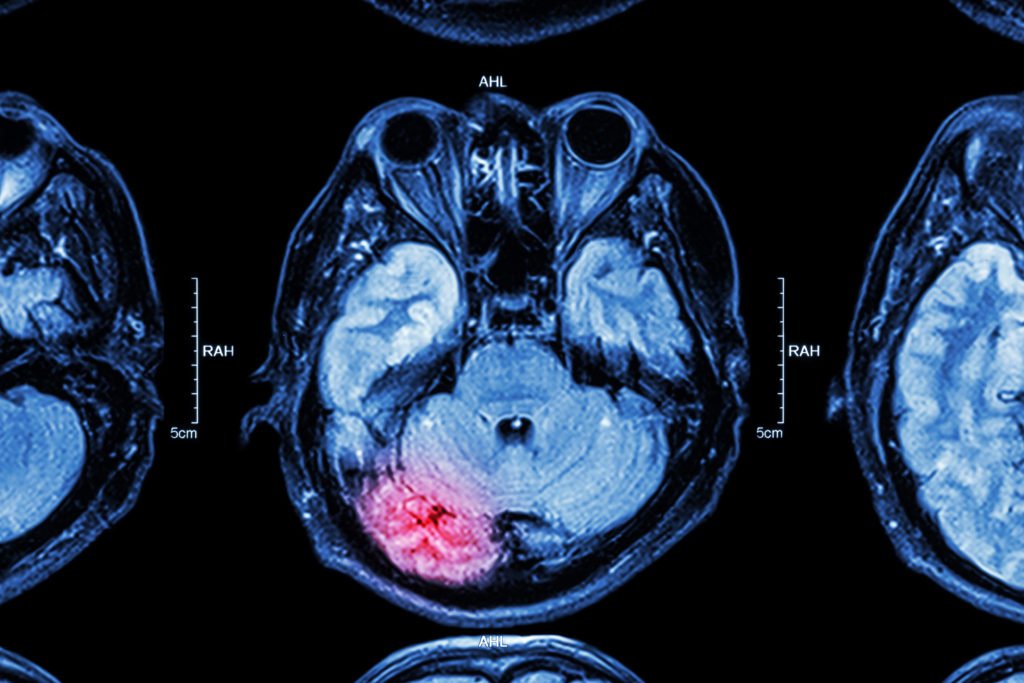
Traumatic brain injury (TBI) is defined as an assault to the brain from an external force that leads to temporary or permanent impairment of cognitive, physical, or psychosocial function. TBI can be open (penetrating) or closed (non-penetrating) and can be categorized as mild, moderate, or severe, depending on the resulting symptomatology. TBI diagnosis is best documented at the time of the injury or within the first 24 hours. During the diagnostic process, a clinician typically assesses the severity of TBI; however, this initial diagnosis does not necessarily predict the extent of disability arising from TBI. The diagnostic process includes neuroimaging, assessing the presence of an altered consciousness or loss of consciousness, assessing the presence of posttraumatic amnesia, and applying the Glasgow Coma Scale score. The Department of Defense (DoD) classifies the severity of TBI using a combination of the four factors mentioned above.
TBI in the U.S. Civilian and Veteran Populations
The Centers for Disease Control and Prevention (CDC) estimates that in 2013, 2.8 million Americans were diagnosed with TBI. Among civilians, TBI accounted for approximately 2.5 million emergency department visits, 282,000 hospitalizations, and 56,000 deaths during that year. The majority of these civilian incidents were due to falls (47 percent) or being struck by or against an object (15 percent).
TBI has been an increasing cause of casualty and disability in the military since the conflicts in Iraq and Afghanistan began. A 2017 Department of Defense and Veterans Brain Injury Center (DVBIC) report estimates that 22 percent of all combat-related casualties from Iraq and Afghanistan are due to TBI. A follow-up DVBIC report from this year estimates that more than 375,000 incidents of TBI were incurred in the military between the years of 2000 and 2018 primarily outside of combat, including training accidents, motor vehicle collisions, and sport-related incidents. Approximately 80 percent of TBI in military personnel are mild in severity, consistent with the civilian population.
Disability Determination Process for Veterans with TBI
Again, the committee was specifically asked to assess the adequacy of the tools and protocols used by VA to provide examinations and also to review the credentials and training of the providers who perform examinations. While the overall adjudication process is not unique to claims for residuals of TBI, there are certain tools and protocols that are specific to those claims that must be addressed.
In Fiscal Year 2017, 155,321 veterans received VA disability compensation for residuals of TBI. VA evaluates residuals of TBI based on the symptoms a veteran is currently experiencing as a result of the trauma, according to an Evaluation of Cognitive Impairment and Other Residuals of TBI not Otherwise Classified, under 38 CFR § 4.12a. VA rates these residuals on a scale of 0, 1, 2, 3, or total, with each of these increments corresponding to a disability rating:
| Scale | Rating |
| 0 | 0% |
| 1 | 10% |
| 2 | 40% |
| 3 | 70% |
| Total | 100% |
VA divides the rating criteria of TBI residuals into 10 subcategories in order to evaluate the condition. Veterans are then rated based on the level of severity and impairment in each of these areas of functioning:
- Memory, attention, concentration, and executive functions
- Judgment
- Social interaction
- Orientation
- Motor activity
- Visual-spatial orientation
- Subjective symptoms
- Neurobehavioral effects
- Communication
- Consciousness
Findings and Conclusions
Healthcare Professionals Trained to Diagnose TBI
The committee reviewed the scientific literature on the natural history of TBI and how it is diagnosed in military personnel, veterans, and civilians in order to comment on the credentials and training necessary for health care specialists to diagnose TBI. Currently, VA requires one of four specialists to diagnose TBI: a neurologist, neurosurgeon, physiatrist, or psychiatrist. The committee found that in addition to those four specialties, there are many specialties and subspecialties involved in making the diagnosis of TBI, particularly if the diagnosis occurs months to years following the injury.
Thus, the committee recommends that VA allows health care professionals who have specific TBI training and experience, in addition to the current required specialists, to make a TBI diagnosis. Additionally, the committee recommends ongoing clinical training that is up to date with the state of current knowledge regarding TBI.
DBQ and VASRD for TBI
Compensation and Pension (C&P) examinations should note the diagnosis and medical nature of the condition and record all requested measurements and test results in a DBQ, which provides limited information that is relevant only to making an evaluation in accordance with the VASRD. Therefore, the structure and content of the DBQ for residuals of TBI is very important. Here, the DBQ criteria mirror those in the section of the VASRD used for rating the residuals of TBI, as the DBQ was developed to aid the non-clinician VA rating specialist in determining the disability rating. The committee reviewed the criteria in the DBQ and VASRD and found that, for the most part, the identified residuals accurately reflect problems that are most likely to disrupt quality of life following TBI. However, some of the characteristics of the criteria used to rate the severity of the disability do not fully capture the residuals’ potential impact. In this way, the DBQ and VASRD fail to take into account some basic medical knowledge concerning how residuals of TBI might manifest and affect disability.
Therefore, the committee recommends that VA convenes experts from both the Veterans Health Administration (VHA) and VBA, including clinicians who diagnose and assess residuals of TBI, to regularly update the VASRD and DBQ for residuals of TBI to better reflect the current state of medical knowledge.
The committee also found that there are important residuals that were completely omitted from the DBQ, including: insomnia, vestibular dysfunction, and near-vision dysfunction. While there are isolated questions on various DBQs related to these symptoms, there is no single DBQ that combines them all in a way that captures the full extent of disability associated with TBI. As such, the committee recommends that VA adds insomnia, vestibular dysfunction, and near-vision dysfunction to the DBQ for residuals of TBI.
Quality of the Adjudication Process
The committee determined that VBA places great emphasis on the consistency of the rating process, rather than on the outcome of the disability determinations. Specifically, the consistency of the rating process was presented as an end in and of itself, rather than as a way of ensuring the reliability and validity of the assessments (i.e. the characteristics of the process needed to ensure that the veteran has been given an accurate disability rating). The committee stated, “a high-quality adjudication process would ideally excel in both of these quality domains, while also being transparent, timely, and credible and minimizing burden to the veteran”. However, the committee also found that transparency was inadequately appreciated as a goal by both VHA and VBA personnel. Accordingly, the committee recommends the following:
- VHA and VBA take specific actions to increase transparency at both individual and system-wide levels, including but not limited to providing veterans with full access to the details of their examinations and ratings, and providing public access to detailed system-wide data on the outcomes of evaluations and outcome quality.
- VA institute processes and programs to measure the reliability and validity of the adjudication process, identify opportunities for improvement in the quality of outcomes, and implement modifications of the adjudication process as needed to optimize quality of both the adjudication process and the reliability and validity of the outcomes.
Overall, these recommendations will allow VA to shift from a focus on the consistency of the process to a focus on the accuracy of the outcome of the evaluation in order to improve the quality of the disability evaluation process for veterans with TBI.
About the Author
Share this Post
