How Does the VA Rate Traumatic Brain Injury (TBI)?
What is a Traumatic Brain Injury (TBI)?
Traumatic brain injury (TBI) can be caused by many factors, such as a blow to the head or an object penetrating the brain, and may result in brain dysfunction. A concussion, for example, is a common form of TBI; however, not all TBIs are concussions.
For the most recent generation of veterans, TBIs are increasingly more widespread due to the increased use of Improvised Explosive Devices (IEDs). Specifically, VA estimates that 22 percent of all combat-related casualties sustained by service members in Iraq and Afghanistan are caused by traumatic brain injuries, a 10 percent increase from rates among Vietnam War veterans.
Common Causes of TBIs
An in-service TBI could result from any sort of blow to the head, but some of the most common causes include IED blasts, combat exposure, motor vehicle accidents, personal assault, or military sexual trauma. Again, traumatic brain injuries have become much more common among veterans who have served in the current conflicts in Iraq and Afghanistan.
VA estimates that 20 percent of all combat-related casualties sustained by troops in Iraq and Afghanistan are brain injuries.
How Are TBIs Diagnosed?
After suffering a TBI, symptoms may begin to manifest cognitively, physically, behaviorally, and/or emotionally. These symptoms of a TBI are unique to the individual and must be evaluated on a case-by-case basis. However, the most common symptoms include the following:
- Dizziness and headaches
- Visual eyesight impairment
- Tinnitus or hearing loss
- Seizures
- Weak muscles
- Stroke or paralysis
- Coordination, balance, and gait disorders
- Difficulty with written and verbal communication
- Impaired memory
- Depression
- Difficulty concentrating
- Poor judgment
TBIs are diagnosed as mild, moderate, or severe based upon medical testing and the severity of the veteran’s symptoms. Residual symptoms of mild TBIs usually, but do not always, resolve within about six months after the injury. Residual symptoms of more acute TBIs can be long-lasting, permanent, or may take years to manifest (e.g. Parkinson’s disease, dementia).
Assessment of a TBI’s initial severity is measured by:
- The results from MRI, PET, CT, or other medical imaging scans
- The length of time that a veteran faced an altered state of consciousness
- The length of time that a veteran remained unconscious
- The length of post-traumatic amnesia
- The score the initial trauma receives on the Glasgow Coma Scale
Below is a table outlining how VA measures the severity of an initial trauma in order to diagnose a TBI:
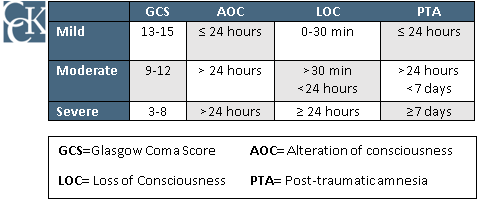
Note: The classification (mild, moderate, severe) measured by the table above has no bearing on VA’s evaluation for a rating decision, only to measure the initial severity of a TBI.
Common Residuals of TBIs
Although mild brain injuries usually resolve themselves within about six months, there can be significant residuals associated with more severe TBIs. Some common residuals that veterans might experience include the following:
- Headaches
- Dizziness
- Visual impairment
- Hearing loss
- Tinnitus
- Seizures
- Muscle weakness
- Inability to complete motor tasks
- Trouble speaking
- Trouble concentrating
- Depression
- Agitation
- Aggression
- Impaired memory
Should Veterans Submit a VA Claim for TBI or Residuals?
Many veterans wonder whether they should file a claim for traumatic brain injury residuals, and the answer is mixed. That is, it depends on what residuals veterans have. Regardless, veterans should consider speaking with an accredited representative or a Veterans Service Organization.
VA should be considering all residuals in its evaluation of a veteran’s TBI; however, if the veteran feels more comfortable filing for a residual condition separately, then they are entitled to do so.
VA Presumptions for Traumatic Brain Injuries
For many years, the VA faced criticism for not recognizing the severity of TBI and the role it plays in facilitating other serious, crippling conditions. It responded to the criticism in 2013 by proposing new regulations that expanded benefits for veterans with TBI who later develop certain conditions. The regulations went into effect in January 2014.
The new regulations presume service connection for five diseases if precipitated by a service-connected TBI. In other words, if you suffered a TBI during your service, the VA must grant service connection to the following:
Parkinson’s disease: Presumed to be service-connected if diagnosed following moderate or severe service-connected TBI.
Seizures: Presumed to be service-connected if diagnosed following moderate or severe service-connected TBI and doctors have established no other cause.
Dementia: Presumed to be service-connected if diagnosed within 15 years of moderate or severe service-connected TBI.
Depression: Presumed to be service-connected if diagnosed within three years of moderate or severe service-connected TBI or within one year of mild TBI.
Hormone Deficiency: Presumed to be service-connected if diagnosed within one year of moderate or severe service-connected TBI.
Compensation & Pension Exams for Traumatic Brain Injuries
After filing a claim for service connection, VA will likely schedule the veteran for an examination. The initial examination will likely be conducted by a neurosurgeon, neurologist, psychiatrist, or psychologist.
How Does VA Rate TBI?
VA evaluates a TBI based on the residual symptoms a veteran is currently experiencing as a result of the trauma, according to an Evaluation of Cognitive Impairment and Other Residuals of TBI not Otherwise Classified, under 38 CFR § 4.124a. VA rates these residuals on a scale of 0, 1, 2, 3, or total, with each of these increments corresponding to a disability rating:
| Scale | Rating |
|---|---|
| 0 | 0% |
| 1 | 10% |
| 2 | 40% |
| 3 | 70% |
| Total | 100% |
VA divides the rating criteria of TBI residuals into 10 subcategories in order to evaluate the condition. Veterans are then rated based on the level of severity and impairment in each of these areas of functioning:
- Impairment of memory, attention, concentration, and executive functions. According to the VA, executive functions include: rate of information processing, setting goals, the ability to plan ahead, prioritizing, problem-solving, decision making, spontaneity, and flexibility in altering unproductive actions or behaviors.
- Altered judgement. Is the veteran able to identify their situation, weigh alternatives, and understand consequences to make reasonable decisions?
- Inhibited social skills. Is the veteran able to act appropriately in social situations?
- Is the veteran aware of: the people around them, their own being, the time and date, where they currently are, and what they are doing there?
- Diminished motor activity (while sensory and motor systems are intact). Such as inhibited intended movement.
- Visual-spatial disorientation. Is the veteran aware of their surroundings? Veterans with visual-spatial disorientation may find it difficult to navigate familiar territory, even with direction.
- Subjective symptoms. Symptoms that cannot be measured with objective tests. A veteran must experience three or more moderate-to-severe subjective symptoms in order to be rated for them. Examples may include, but are not limited to, depression and anxiety.
- Neurobehavioral effects. These can include irritability, unpredictability, impulsivity, verbal aggression, lack of cooperation, and impaired awareness of disability.
- Worsened ability to communicate. This includes communication by spoken or written word, as well as the ability to comprehend spoken and written language.
- Is the veteran conscious, in a coma, or in a vegetative state?
Overlapping Symptoms: Mental Health Conditions and TBIs
Many mental health conditions can overlap with TBI symptomology, but it is important to note that the same symptoms cannot be used to rate two separate disorders. A veteran’s symptoms cannot be linked to a previously rated condition if they are to be considered as part of the rating for a traumatic brain injury.
For instance, if you receive a 100 percent disability rating for your depression under the TBI rating criteria, you cannot also be separately rated at 100 percent for your depression. In other words, if veterans experience both mental health and TBI symptomology VA will only provide one disability rating. Pyramiding is the VA term for rating the same disability – or same manifestation (i.e., symptom) of a disability – twice.
Does VA Rate Traumatic Brain Injuries Accurately?
VA often under-rates TBIs. In many cases, VA will rely on Compensation & Pension examinations and overlook veteran’s lay testimony. Veterans may have to appeal VA’s decisions in order to obtain a higher disability rating.
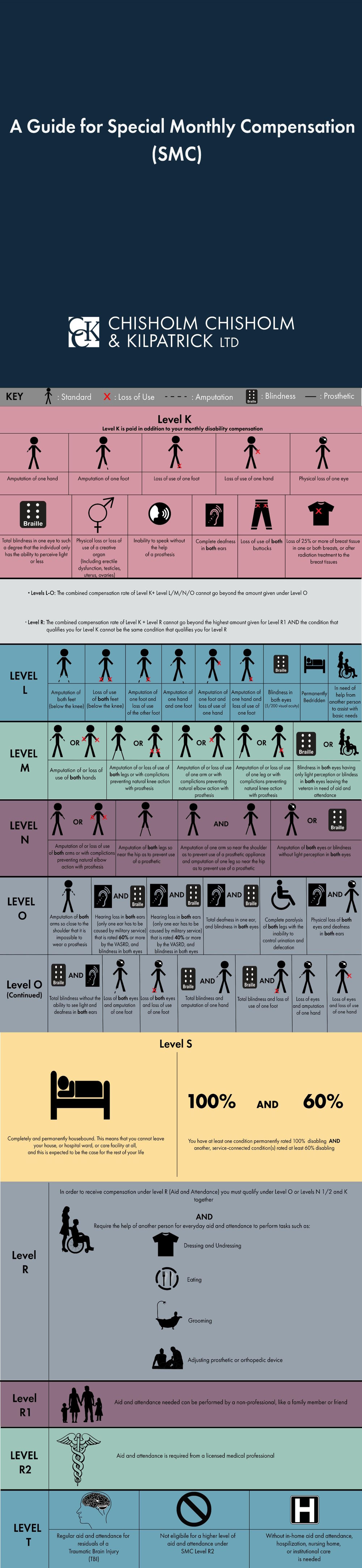
Can My TBI Qualify Me for Special Monthly Compensation (SMC)?
VA established a level of special monthly compensation (SMC), referred to as SMC(t) specifically for veterans who have experienced a severe TBI. SMC(t) shares the monthly compensation amount of SMC(r-2), but without the strict requirements needed to qualify for SMC(r-2). A veteran’s service-connected TBI qualifies them to receive SMC(t) if:
- They are in need of regular aid and attendance (A&A) due to the residuals of TBI. A&A is characterized by a veteran’s inability to dress, bathe, feed, use the restroom, or avoid exposure to hazards in daily life by themselves.
- They would otherwise require residential institutional care (i.e. hospitalization or nursing home) if they did not receive regular, in-home A&A.
- They do not qualify for a higher level of A&A under SMC(r-2).
What If I Cannot Work Due to My TBI?
Veterans who are unable to secure and follow substantially gainful employment as a result of their TBI may qualify for Total Disability based on Individual Unemployability (TDIU). TDIU allows veterans to be compensated at the 100 percent rate, even if their conditions do not combine to equal a 100 percent schedular rating.
How Much Can I Receive in VA Disability for a Traumatic Brain Injury (TBI)?
The VA uses a rating schedule to determine disability benefit amounts. To determine your rating, the VA evaluates the residual emotional/behavioral, physical, and cognitive dysfunction that resulted from your TBI. This can be complex as there can be several different injuries and ratings related to your TBI.
As of December 1st, 2023 the VA disability rate benefit amounts are as follows:
- 0 percent disability rating: $0.00 per month
- 10 percent disability rating: $171.23 per month
- 20 percent disability rating: $338.49 per month
- 30 percent disability rating: $524.31 per month
- 40 percent disability rating: $755.28 per month
- 50 percent disability rating: $1,075.16 per month
- 60 percent disability rating: $1,361.88 per month
- 70 percent disability rating: $1,716.28 per month
- 80 percent disability rating: $1,995.01 per month
- 90 percent disability rating: $2,241.91 per month
- 100 percent disability rating: $3,737.85 per month
If you have dependents in your household, such as a spouse, children, or dependent parents, you can receive benefits on their behalf with a disability rating of 30 percent or higher. A separate schedule from the VA shows your benefit amount based on the number of dependents in your household.
Call Chisholm Chisholm & Kilpatrick LTD for a Free Case Evaluation
If you are a veteran suffering from a TBI and its residuals, you may be eligible to receive disability compensation from VA. If your TBI claim has been denied, Chisholm Chisholm & Kilpatrick LTD may be able to help you file an appeal. Call 800-544-9144 for a free case evaluation.
About the Author
Share this Post